Every night, while you sleep, your body might be fighting for air. If you have obstructive sleep apnea (OSA), your airway collapses repeatedly-sometimes dozens of times an hour-cutting off oxygen just long enough to jolt your brain awake. You may not remember it, but your heart feels every one of those moments. And over time, those silent interruptions are quietly raising your risk of high blood pressure, irregular heartbeats, heart failure, and stroke.
What Happens to Your Heart During Sleep Apnea?
When your airway closes during sleep, your oxygen levels drop. Your body doesn’t like that. It triggers an emergency response: your nervous system goes into overdrive. Your heart rate spikes, your blood pressure surges by 20 to 40 mmHg, and your body releases stress hormones. This isn’t a one-time event. In severe cases, it can happen 50, 60, or even 100 times a night. Each time, your heart gets slammed with pressure and strain.This isn’t just about being tired in the morning. These repeated stress events damage the lining of your blood vessels, cause inflammation, and make your blood more likely to clot. Over months and years, that adds up. Studies show people with severe sleep apnea (more than 30 breathing pauses per hour) have a 40-50% higher chance of having a heart attack, stroke, or other major cardiovascular event compared to those without it.
Why Blood Pressure Won’t Stay Down
If you’re on medication for high blood pressure but still can’t get your numbers under control, sleep apnea might be the hidden reason. About 30-40% of people with high blood pressure also have undiagnosed OSA. And it’s not just because they’re overweight-research confirms that even after accounting for obesity, diabetes, and other factors, OSA independently raises blood pressure.Here’s how it works: during each apnea, your body’s fight-or-flight response kicks in. Your sympathetic nervous system fires up, squeezing your blood vessels tighter. When you finally breathe again, your blood rushes back into your heart with a sudden surge. That back-and-forth-tightening, then flooding-wears down your arteries and forces your heart to work harder, even during the day.
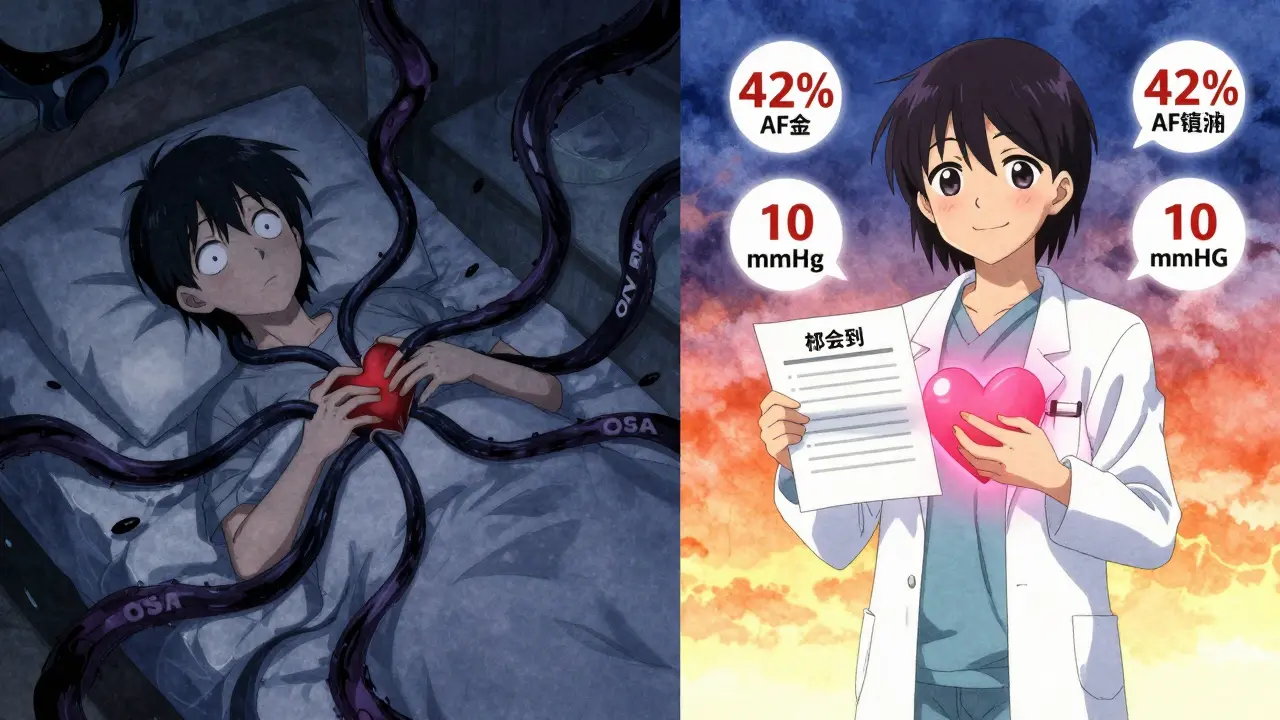
Studies show that using CPAP therapy for just 4 hours a night can lower systolic blood pressure by 5-10 mmHg on average. That’s the same drop you’d expect from a second blood pressure pill. For many people, that’s enough to reduce or even eliminate the need for medication.
Arrhythmias: When Your Heart Goes Off Rhythm
Your heart doesn’t just beat harder-it starts beating erratically. Sleep apnea is one of the strongest known triggers for atrial fibrillation (AFib), the most common type of irregular heartbeat. People with OSA are 3 to 5 times more likely to develop AFib than those without it. In fact, severe sleep apnea increases AFib risk by 140%, which is higher than the risk from high blood pressure alone.Why? Because the repeated drops in oxygen and spikes in stress hormones create electrical chaos in the heart’s upper chambers. The heart muscle becomes scarred and stiff over time, making it easier for abnormal signals to start and spread. One 2024 study using cardiac MRI found that OSA patients had more than twice the amount of scar tissue in their atria compared to healthy controls.
And it’s not just AFib. Sleep apnea also increases the risk of other arrhythmias, including ventricular tachycardia and bradycardia. Even if you’ve had a successful heart procedure like an ablation for AFib, if your sleep apnea goes untreated, your chances of the arrhythmia coming back are nearly twice as high.

It’s Not Just Older People
For years, doctors thought sleep apnea was mainly a problem for middle-aged, overweight men. But new research from UT Southwestern Medical Center (2024) shows that even adults under 40 with untreated OSA face a significantly higher risk of heart disease. Younger patients may not have other risk factors like high cholesterol or diabetes, but the mechanical stress from repeated breathing stops is enough to damage the heart on its own.This means if you’re under 40, snore loudly, wake up gasping, or feel exhausted even after a full night’s sleep-you could be at risk. Age doesn’t protect you. If your heart is acting up, your sleep might be the missing piece.
What Treatment Actually Does
The good news? Treating sleep apnea reverses much of the damage. Continuous Positive Airway Pressure (CPAP) therapy keeps your airway open while you sleep. It’s not perfect-some people struggle with the mask, the noise, or the feeling of air pressure-but for those who stick with it, the results are clear.After 12 months of consistent CPAP use (at least 4 hours a night), studies show:
- A 42% reduction in atrial fibrillation recurrence
- A 5-10 mmHg drop in systolic blood pressure
- A 65% chance of needing fewer blood pressure medications
- 78% report better daytime energy and focus
One user on the American Heart Association’s support forum shared: “After six months of CPAP, my AFib episodes dropped from weekly to once every two or three months.” Another, diagnosed with severe OSA (AHI of 42), saw his blood pressure fall from 160/95 to 128/82 in just three months.
For those who can’t tolerate CPAP, alternatives like oral appliances or hypoglossal nerve stimulation (like the Inspire device) are now available. The Inspire system, implanted like a pacemaker, stimulates the nerve that controls the tongue to keep the airway open. In clinical trials, it reduced apnea events by 79% and improved daytime sleepiness by 68%.
Who Should Be Screened?
You don’t need to wait for symptoms to get worse. Major medical groups now recommend screening for sleep apnea if you have:- High blood pressure (especially if it’s hard to control)
- Atrial fibrillation or other arrhythmias
- Heart failure
- Had a stroke or transient ischemic attack (TIA)
- Snore loudly, wake up gasping, or feel tired despite sleeping 8 hours
Here’s the shocking part: 45-65% of people with these conditions have undiagnosed sleep apnea. Yet only 20-25% of at-risk patients are even tested in primary care.
Testing is easier than ever. Home sleep apnea tests are now accurate for most people and cost a fraction of an overnight hospital stay. Insurance, including Medicare, covers these tests if you have symptoms or conditions linked to OSA.
Don’t Wait for a Heart Event
Sleep apnea doesn’t just cause snoring. It’s a silent, nightly assault on your heart. Every time you stop breathing, your heart pays the price. Left untreated, it can lead to permanent damage-scarred heart tissue, stubborn high blood pressure, and life-threatening arrhythmias.But here’s the best part: unlike genetic risks or aging, sleep apnea is treatable. And the earlier you treat it, the more you can protect your heart. If you’ve been told your blood pressure won’t budge, or your arrhythmia keeps coming back, ask: could sleep apnea be the reason? A simple test could change your heart’s future.