Medication Side Effect Risk Calculator
Genetic Risk Assessment
Drug Interaction Check
Personalized Recommendations
Select your genetic factors and medications to see personalized advice.
Why This Matters
Your body's reaction to medications depends on how your genes process drugs and how drugs interact with each other. 75-80% of side effects are predictable based on these factors.
Ever taken a pill and felt weird afterward? Nausea, dizziness, a rash, or even just feeling "off"-you’re not alone. About 75-80% of all side effects from medications are predictable, not random. They happen because drugs don’t just target the problem area-they interact with your whole body in ways scientists are still mapping out.
What Exactly Is a Side Effect?
A side effect, or adverse drug reaction (ADR), is any unwanted effect that happens when you take a medicine. It’s not a mistake. It’s biology. The FDA defines it as any response to a drug that’s noxious, unintended, and occurs at normal doses. Think of it like a key that fits the right lock (your target), but also jiggles a few other locks nearby. That’s how most side effects start.Why Your Body Reacts: The Two Big Reasons
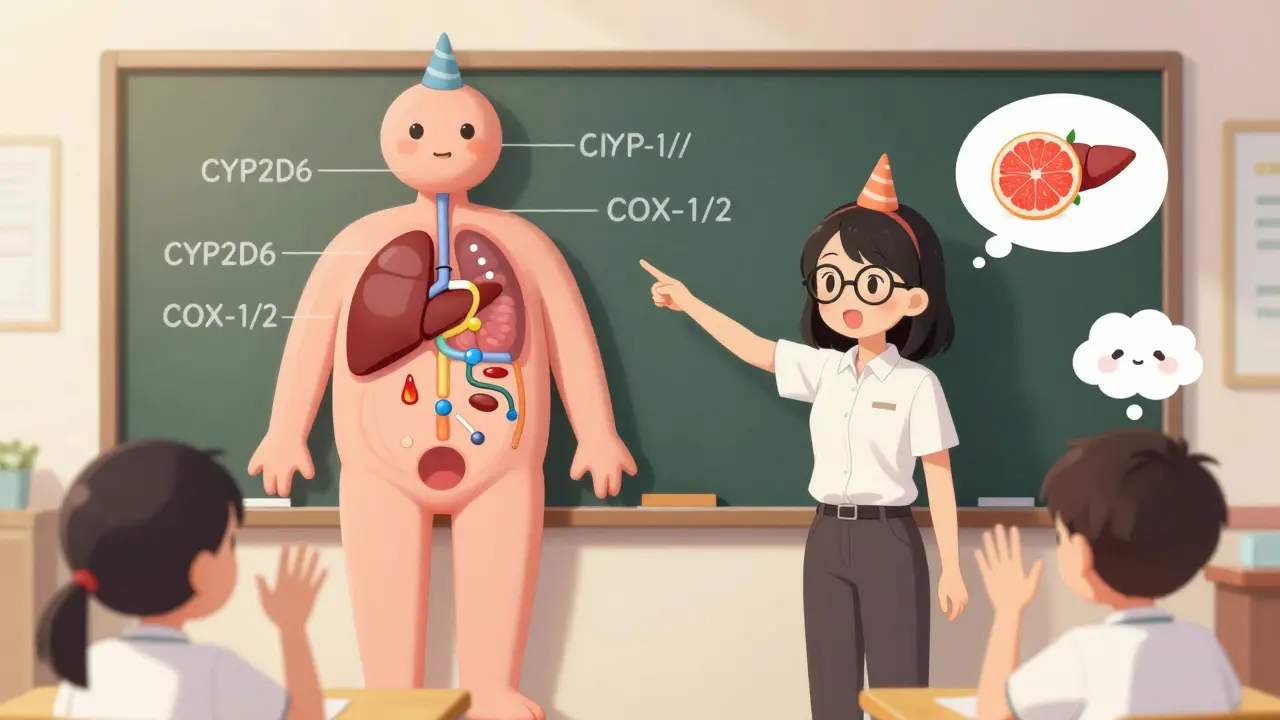
There are two main reasons medications cause side effects: how your body handles the drug (pharmacokinetics) and how the drug interacts with your body (pharmacodynamics).Pharmacokinetics is about absorption, distribution, metabolism, and excretion. Your liver breaks down most drugs using enzymes called cytochrome P450. But here’s the catch: not everyone has the same version of these enzymes. About 5-10% of people of European descent have a slow version of CYP2D6. That means if they take codeine, their body turns it into morphine too slowly-or too quickly-leading to dangerous breathing problems. It’s not the drug’s fault. It’s your genes.
Pharmacodynamics is about what the drug does to your body. Take NSAIDs like ibuprofen. They reduce pain by blocking COX-2, the enzyme tied to inflammation. But they also block COX-1, which protects your stomach lining. That’s why 15-30% of regular users end up with stomach irritation or ulcers. The drug didn’t "go rogue." It just hit two targets instead of one.
Off-Target Effects: When Drugs Hit the Wrong Spot
Many drugs aren’t perfectly precise. Haloperidol, used to treat psychosis, works by blocking dopamine in the brain. But dopamine receptors are also in the basal ganglia, which control movement. So 30-50% of people on haloperidol develop tremors, stiffness, or involuntary movements within days. It’s not a flaw in the patient-it’s a flaw in the drug’s design.Even weirder: some drugs don’t even need to bind to a protein to cause trouble. A 2021 study from Weill Cornell Medicine showed that drugs that interact with cell membranes-like antibiotics or antifungals-can change the membrane’s thickness or flexibility. That messes up proteins embedded in the membrane, even if the drug never touches them directly. Think of it like shaking a table and watching all the glasses wobble. The drug didn’t touch the glasses, but they moved anyway.
Immune System Reactions: When Your Body Turns Against the Drug
About 20-25% of side effects are unpredictable and tied to your immune system. These aren’t allergies in the traditional sense, but they can feel like it.Type I reactions happen fast-within minutes. Penicillin can trigger anaphylaxis in 1-5 out of every 10,000 courses. That’s rare, but deadly. Type IV reactions are slower. They’re T-cell driven and can show up weeks later. Stevens-Johnson Syndrome, a severe skin reaction, is linked to drugs like allopurinol and sulfonamides. It affects 1-6 people per million each year, but when it happens, it’s life-threatening.
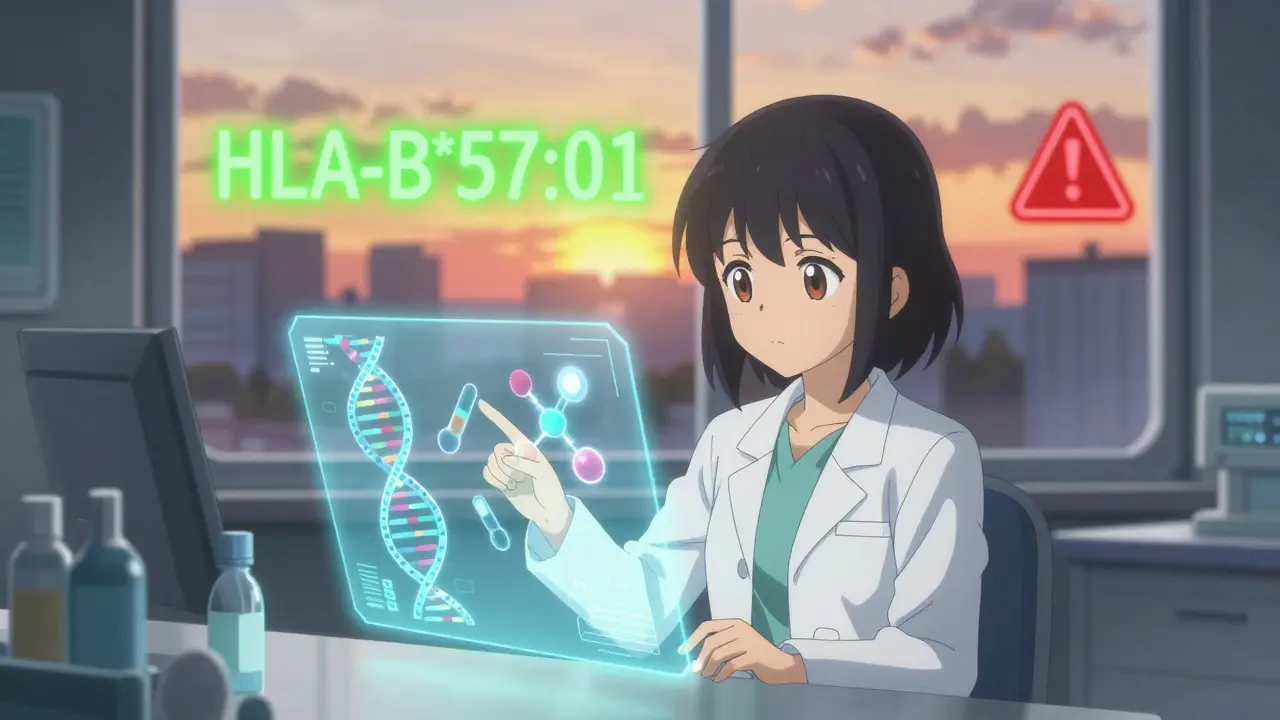
Then there’s the HLA-B*57:01 gene. If you have it, your risk of a dangerous reaction to abacavir (an HIV drug) jumps 50 to 100 times. That’s why doctors now test for this gene before prescribing abacavir. Since screening started, reactions dropped from 5-8% to under 0.5%.
Drug Interactions: When Two Medicines Collide
Taking multiple drugs increases side effects dramatically. One drug can change how another works. Grapefruit juice, for example, blocks the enzyme CYP3A4. That means if you’re on felodipine (a blood pressure drug), grapefruit can spike your blood levels by 260%. Result? Dangerous drops in blood pressure.Rifampicin, an antibiotic, speeds up the breakdown of digoxin, a heart medication. That can lower digoxin levels by 30-50%, making it useless. NSAIDs reduce blood flow to the kidneys, which slows down methotrexate clearance. That can lead to bone marrow failure.
In older adults taking five or more medications, drug interactions cause 6-7% of hospital admissions. That’s not just bad luck-it’s a system failure.
How Doctors Fight Back
We’re not helpless. Science is giving doctors better tools.Genetic testing is now routine for some drugs. Before prescribing abacavir, they test for HLA-B*57:01. Before giving clopidogrel (a blood thinner), they check CYP2C19 status. Poor metabolizers get an alternative-no more risk of heart attack from a useless drug.
Therapeutic drug monitoring keeps levels in the safe zone. Digoxin, for example, is kept between 0.5 and 0.9 ng/mL. Too low? Ineffective. Too high? Toxic.
Prophylactic meds help too. If you’re on long-term NSAIDs and have a history of ulcers, your doctor may give you a proton pump inhibitor. That cuts ulcer risk by 70-80%.
Dose titration is simple but powerful. Starting an SSRI at a low dose reduces nausea and dizziness in 20-30% of patients. Slow and steady wins the race.
What’s Next? Smarter Drugs, Smarter Systems
The future is about prediction. The FDA’s Sentinel Initiative tracks 300 million patient records in real time. That’s how they spotted that pioglitazone increased heart failure risk by 1.5 to 2 times. No clinical trial caught that. Real-world data did.Artificial intelligence is now being used to predict off-target effects before a drug even hits the lab. A 2023 study in Nature Reviews Drug Discovery found AI could cut late-stage trial failures due to toxicity by 25-30%. That’s billions saved-and more drugs reaching patients safely.
Researchers at Weill Cornell are now building models to predict which membrane proteins are most vulnerable to drug-induced changes. That could lead to drugs that don’t just work better-but cause fewer side effects from day one.
Bottom Line: Side Effects Aren’t Random
Side effects aren’t a bug. They’re a feature of biology. Every drug is a molecule with a specific shape, trying to fit into a body made of trillions of moving parts. Sometimes, it fits too well-or not well enough.The good news? We’re getting better at seeing it coming. Genetic tests, real-time monitoring, smarter prescribing, and AI-driven design are turning side effects from a gamble into a manageable risk. You still might feel a little off after taking a new pill. But now, doctors have more tools than ever to figure out why-and how to fix it.