When you pick up a prescription at the pharmacy, you might not think twice about whether you’re getting the brand-name drug or a cheaper generic. But behind that decision is a detailed, science-backed system the FDA uses to decide if those generics are truly interchangeable. This system is called therapeutic equivalence codes, and it’s the reason pharmacists can swap out brand-name drugs for generics without asking your doctor every time.
What therapeutic equivalence really means
Therapeutic equivalence isn’t just about having the same active ingredient. It means two drugs - one brand, one generic - will work the same way in your body, with the same safety and effectiveness. The FDA doesn’t just assume this. They require proof. For a generic drug to be rated as therapeutically equivalent, it must meet three strict criteria:- It has the same active ingredient, strength, dosage form, and route of administration as the brand-name drug (this is called pharmaceutical equivalence).
- It has been shown through testing to deliver the same amount of drug into your bloodstream at the same rate (this is bioequivalence).
- It has the same safety and clinical effect under the conditions listed in the drug’s labeling.
Only drugs that pass all three tests get an ‘A’ rating. That’s the green light for substitution. If a drug doesn’t meet one of these standards, it gets a ‘B’ rating - meaning it’s not automatically interchangeable.
The Orange Book: The FDA’s official drug substitution guide
The FDA publishes all this information in a document called the Approved Drug Products with Therapeutic Equivalence Evaluations - better known as the Orange Book. It’s been around since 1980, and every month, it’s updated with new generic approvals, code changes, and withdrawn products.Pharmacists, doctors, and state pharmacy boards rely on the Orange Book daily. In 2023, it listed over 14,000 approved drug products. About 90% of them - nearly 12,600 - have an ‘A’ rating. That’s why generic drugs make up 90% of all prescriptions filled in the U.S., but only cost 23% of the total drug spending.
It’s not just a reference guide - it’s the legal backbone for substitution laws. In 49 states, pharmacists can switch a brand-name drug for an ‘A’-rated generic without needing to call your doctor. That saves time, money, and reduces delays in getting treatment.
Decoding the letters: What A, B, AB1, BC, and BX really mean
The codes aren’t random. They’re a shorthand system that tells you exactly what you’re dealing with.- A = Therapeutically equivalent. Safe to substitute.
- B = Not rated as equivalent. Don’t substitute unless your doctor says so.
But it gets more specific. After the first letter, additional letters give more detail:
- AB = The generic meets all bioequivalence standards. Most common ‘A’ code.
- AB1, AB2, AB3, AB4 = Used when multiple brand-name drugs serve as reference points. For example, if two different brand versions of the same drug exist, generics are matched to each one separately. AB1 means it’s equivalent to the first reference drug; AB2 to the second, and so on.
- BC = Extended-release products with bioequivalence concerns. These often get ‘B’ ratings because their slow-release mechanism is hard to replicate exactly.
- BT = Topical products like creams or gels where skin absorption is inconsistent.
- BN = Aerosol or nebulizer products - tricky because delivery depends on device design.
- BX = Not enough data to decide. These are usually new generics or complex drugs still under review.
Here’s the catch: A ‘B’ rating doesn’t always mean the drug is unsafe or ineffective. It just means the FDA doesn’t have enough proof to say it’s interchangeable. For example, some topical creams or inhalers may work just fine in practice, but the current testing methods can’t reliably prove bioequivalence. That’s why some doctors and pharmacists get confused.
Why some generics get ‘B’ codes - and why it matters
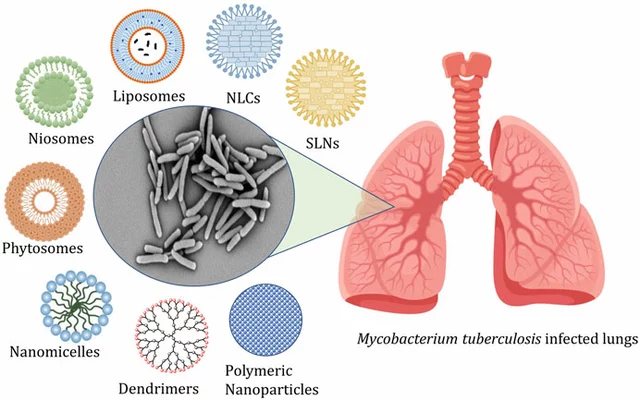
Complex drug products are the biggest challenge for the TE code system. Think of things like inhalers, injectables, or topical ointments. These aren’t just pills you swallow. Their effectiveness depends on how they’re delivered - the device, the particle size, the way they stick to skin or lung tissue.Standard blood tests can’t always show if two inhalers deliver the same amount of medicine to the lungs. So even if two products are clinically the same, the FDA may still assign a ‘B’ code because the current bioequivalence methods aren’t good enough.
Between 2018 and 2022, the number of ‘B’-rated applications for complex generics rose by 22%. That’s not because more products are failing - it’s because more complex products are being developed. The FDA admits this is a gap. In its 2022 draft guidance, they proposed new ways to evaluate these drugs, including better in vitro tests and real-world data.
Meanwhile, pharmacists are stuck in the middle. A 2022 survey by the American Medical Association found that 42% of physicians didn’t understand how to interpret ‘B’ codes. And 28% reported cases where pharmacists refused to substitute a ‘B’-rated drug - even when it was the right choice for the patient.
How pharmacists use TE codes in real life
For pharmacists, the Orange Book is part of daily work. According to a 2022 survey by the National Community Pharmacists Association, 87% of pharmacists say TE codes make substitution faster and easier. About 73% check the Orange Book at least once a week.On average, pharmacists spend 2.7 minutes per prescription verifying the TE code. That adds up. The American Pharmacists Association estimates this system saves the U.S. healthcare system $1.2 billion a year by enabling safe generic substitution.
But it’s not foolproof. In 38 states, pharmacists are required to notify the prescribing doctor if they substitute a ‘B’-rated product. Some states require written documentation. Others require the patient to sign a form. The rules vary - which is why pharmacists need to know not just the code, but their state’s laws too.
How the system compares to other countries
The U.S. system is unique. The European Medicines Agency (EMA) doesn’t use codes like ‘A’ or ‘B’. Instead, they publish detailed scientific reviews for each generic application. It’s thorough - but not practical for daily pharmacy use.In the U.S., a pharmacist can glance at the Orange Book and know instantly if they can swap a drug. In Europe, they’d need to read through pages of technical data. The FDA’s system is designed for speed and clarity - which works well for simple oral tablets, but struggles with complex delivery systems.
What’s changing in 2025 and beyond
The FDA is working to modernize the system. Their 2023-2027 strategic plan aims to reduce ‘B’ ratings for complex generics by 30% by 2027. They’re expanding their Product-Specific Guidance documents - now over 1,850 - to give drugmakers clearer rules on how to prove bioequivalence for tricky products.Future updates may include real-world evidence - like data from patient outcomes, electronic health records, or pharmacy claims - to supplement traditional lab tests. This could help classify complex generics like inhalers or injectables more accurately.
For now, the system works. It’s saved billions, kept patients safe, and made generics accessible. But as drug technology gets more advanced, the FDA’s code system will need to evolve too.
Frequently Asked Questions
Can I ask my pharmacist to give me the brand-name drug instead of the generic?
Yes. Even if a generic has an ‘A’ rating, you can request the brand-name version. Your pharmacist must honor that request, though you may pay more. Some insurance plans require you to try the generic first before covering the brand.
Are over-the-counter (OTC) drugs rated with therapeutic equivalence codes?
No. The FDA’s therapeutic equivalence system only applies to prescription drugs. OTC medications like ibuprofen or antacids are not assigned TE codes, even though many have generic versions. Substitution for OTC drugs is left to the discretion of the consumer and retailer.
What does it mean if my prescription says "Do Not Substitute"?
That means your doctor has specifically requested the brand-name drug - either because of clinical reasons or past experience with your response to that specific product. Pharmacists are legally required to follow this instruction, even if a generic has an ‘A’ rating. The TE code doesn’t override the prescriber’s direction.
Why do some generics cost more than others even if they have the same TE code?
Price differences come from manufacturing costs, distribution deals, and market competition - not therapeutic equivalence. Two generics with the same AB rating might be made by different companies, have different packaging, or be sold under different distribution agreements. The FDA doesn’t control prices - only safety and effectiveness.
How often are TE codes updated?
The FDA updates the Orange Book monthly. New generic approvals, withdrawn products, and code changes (like switching a B to an A) are added as soon as they’re finalized. Pharmacists and pharmacies typically sync their databases weekly to stay current.
What to do next
If you’re a patient: Check your prescription label. If it says “substitution permitted,” your pharmacist can switch to a generic with an ‘A’ rating. If you’re unsure, ask your pharmacist to show you the TE code in the Orange Book - they’re trained to explain it.If you’re a prescriber: Always use clear language. If you don’t want substitution, write “Dispense as written” or “Do Not Substitute.” Don’t rely on vague terms like “brand necessary.”
If you’re a pharmacist: Always verify the TE code before substituting. Use the FDA’s official Orange Book website - not third-party apps - for the most accurate, up-to-date ratings. When in doubt about a ‘B’ code, contact the prescriber.
The system isn’t perfect, but it’s working. It’s kept millions of Americans on affordable, effective medication for over 40 years. Understanding how it works helps you make better choices - whether you’re taking a pill, filling a prescription, or just wondering why your medication costs less this month.