Vitamin D Dosing Calculator for Thyroid Patients
This calculator provides personalized vitamin D dosing recommendations based on current serum 25(OH)D levels and thyroid health guidelines. For best results, use with your lab results and under medical supervision.
Recommended Dosing
Note: These are general guidelines. Always consult your healthcare provider before starting supplementation. Monitor levels every 3-6 months.
When you hear the word "thyroid deficiency," most people think of hormone replacement pills and regular blood tests. Rarely do they connect it to a simple sunshine vitamin. Yet a growing body of research shows that vitamin D can influence thyroid function, auto‑immune activity, and overall symptom relief. This guide walks you through what you need to know-why the link matters, how to test, which doses work, and what pitfalls to avoid-so you can make an informed decision about adding vitamin D to your thyroid care plan.
Quick Takeaways
- Low serum 25(OH)D is common in people with hypothyroidism and autoimmune thyroid disease.
- Vitamin D supports immune regulation, reducing the odds of thyroid‑autoantibody spikes.
- Target serum 25(OH)D levels: 30‑50 ng/mL for most thyroid patients.
- Typical supplementation: 1,000-4,000 IU daily, adjusted based on baseline labs.
- Monitor TSH, FT4, and calcium levels every 3‑6 months while supplementing.
Understanding Thyroid Deficiency
Thyroid deficiency is a condition where the thyroid gland fails to produce enough hormones, mainly thyroxine (T4) and triiodothyronine (T3). The shortfall leads to a slowed metabolism, fatigue, weight gain, and cold intolerance. The most common medical label is hypothyroidism, which can be primary (gland‑related) or secondary (pituitary‑related).
Autoimmune attacks, especially Hashimoto's thyroiditis, account for roughly 80 % of hypothyroid cases in developed countries. In Hashimoto’s, the immune system produces antibodies-thyroid peroxidase (TPO) and thyroglobulin (Tg)-that damage the thyroid tissue over time.
Standard management involves levothyroxine replacement, regular monitoring of thyroid‑stimulating hormone (TSH) and free T4 (FT4), and lifestyle tweaks. But the endocrine system does not operate in isolation; nutrients, especially vitamin D, can modulate the immune environment that fuels auto‑immunity.
Why Vitamin D Matters for the Thyroid
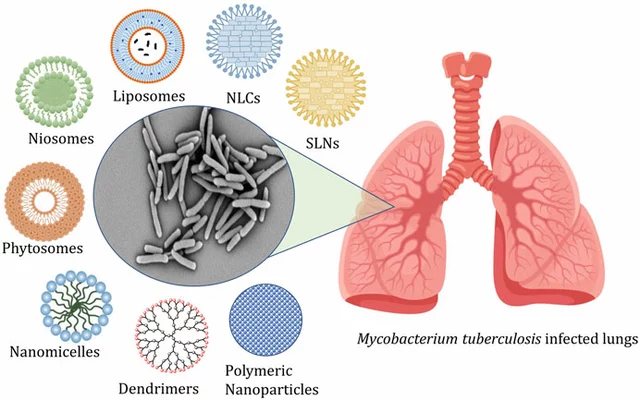
Vitamin D is a fat‑soluble nutrient that functions as a hormone. After skin synthesis or dietary intake, it is converted to 25‑hydroxyvitamin D (25(OH)D) in the liver, then to the active form 1,25‑dihydroxyvitamin D in the kidneys. The active form binds the vitamin D receptor (VDR) present in many cells, including immune cells and thyroid follicular cells.
Three mechanisms explain the connection:
- Immune modulation: Vitamin D shifts T‑cell responses from pro‑inflammatory Th1/Th17 toward regulatory T‑cells (Tregs). This balance dampens the autoimmune assault on the thyroid.
- Calcium‑parathyroid interplay: Low vitamin D can trigger secondary hyperparathyroidism, raising parathyroid hormone (PTH) levels that interfere with thyroid hormone conversion.
- Gene expression: VDR activation influences genes involved in thyroid hormone synthesis, potentially improving the gland's residual capacity.
Observational studies from 2022‑2024 consistently report that 60‑70 % of patients with Hashimoto’s have serum 25(OH)D below 20 ng/mL, a threshold considered deficient. Randomized trials show that correcting this deficiency can reduce TPO antibody titers by 15‑30 % after six months of supplementation.
Assessing Vitamin D Status in Thyroid Patients
The gold‑standard test is the serum 25‑hydroxyvitamin D level, reported in nanograms per milliliter (ng/mL) or nanomoles per liter (nmol/L). Here’s a practical reference:
- Deficient: < 20 ng/mL (< 50 nmol/L)
- Insufficient: 20‑30 ng/mL (50‑75 nmol/L)
- Optimal for thyroid health: 30‑50 ng/mL (75‑125 nmol/L)
- Potential toxicity: > 100 ng/mL (> 250 nmol/L)
When ordering labs, ask your clinician to include TSH, FT4, calcium, and PTH alongside 25(OH)D. This comprehensive panel helps identify whether low vitamin D is merely a co‑factor or part of a broader endocrine imbalance.
Supplementation Strategies Tailored to Thyroid Deficiency
Once a deficiency is confirmed, the goal is to raise serum 25(OH)D into the optimal range without overshooting. Below is a typical dosing algorithm, adjusted for body weight and baseline levels:
| Baseline 25(OH)D (ng/mL) | Loading Dose (IU/week) | Maintenance Dose (IU/day) |
|---|---|---|
| <20 | 50,000 IU once weekly for 8 weeks | 2,000‑4,000 IU daily |
| 20‑30 | 50,000 IU once weekly for 4 weeks | 1,500‑2,500 IU daily |
| 30‑50 (target range) | - | 1,000‑1,500 IU daily |
Key points:
- Choose cholecalciferol (vitamin D3) over ergocalciferol (D2) for better bioavailability.
- Take the supplement with a fatty meal to maximize absorption.
- Re‑test serum 25(OH)D after 8‑12 weeks of loading, then every 3‑6 months.
- If calcium rises above 10.5 mg/dL or PTH spikes, reduce the dose and investigate other causes.
Dietary Sources & Lifestyle Tips
While supplements are the fastest way to correct deficiency, food and sun exposure play supporting roles.
- Fatty fish: salmon, mackerel, sardines (300‑400 IU per 3‑oz serving).
- Fortified products: dairy, plant milks, orange juice (100‑150 IU per cup).
- Mushrooms exposed to UV light: up to 400 IU per ½ cup.
- Sunlight: 10‑15 minutes of midday sun on arms and face (latitude 35°‑45°) can generate 1,000‑2,000 IU, but sunscreen, skin tone, and season dramatically affect output.
For Canadian residents like those in Ottawa, the winter months often yield vitamin D synthesis rates of less than 200 IU per day. That makes a year‑round supplement almost mandatory for thyroid patients.
Potential Pitfalls & Safety Concerns
Vitamin D is safe at recommended doses, but excess intake can cause hypercalcemia, kidney stones, and vascular calcification. Watch out for:
- High‑dose prescription forms (>10,000 IU/day) without lab monitoring.
- Concurrent use of calcium supplements that push total calcium intake beyond 2,500 mg/day.
- Underlying granulomatous diseases (e.g., sarcoidosis) that increase conversion to the active form, raising toxicity risk.
Always discuss any new supplement regimen with your endocrinologist, especially if you take medications that affect calcium metabolism (like thiazide diuretics) or are on anticoagulants.

Monitoring & Follow‑Up
Effective management is a loop:
- Baseline labs: 25(OH)D, TSH, FT4, calcium, PTH.
- Start supplementation based on the dosing guide.
- Re‑test 25(OH)D in 8‑12 weeks; adjust dose if still below 30 ng/mL.
- Every 3‑6 months, repeat the full panel to ensure thyroid function remains stable and calcium stays within range.
- If TPO antibodies drop significantly, consider tapering levothyroxine dose under medical supervision.
Documentation of symptom changes-energy levels, weight, mood, and temperature tolerance-helps correlate lab results with real‑world outcomes.
Putting It All Together: A Sample 12‑Month Plan
Below is an illustrative timeline for a 45‑year‑old patient with Hashimoto’s, baseline 25(OH)D = 15 ng/mL, TSH = 6.5 mIU/L, and normal calcium.
- Month 0: Order labs; start loading dose 50,000 IU weekly.
- Month 2: Re‑check 25(OH)D; expected rise to ~35 ng/mL. Switch to maintenance 2,000 IU daily.
- Month 4: Full panel; TSH may drop to 4.0 mIU/L, TPO antibodies down 12 %.
- Month 6: Add 1,000 IU vitamin D‑rich fish meals twice weekly; monitor calcium.
- Month 9: Re‑test; if 25(OH)D stable at 40‑45 ng/mL, maintain current dose.
- Month 12: Comprehensive review; consider modest levothyroxine reduction if TSH < 3.0 mIU/L and symptoms improved.
Each step is guided by lab data, not guesswork, ensuring safety and maximizing benefit.
Final Thoughts
Vitamin D isn’t a magic cure, but it’s a powerful adjunct in thyroid deficiency management. By normalizing vitamin D status, you can calm the immune system, stabilize calcium‑parathyroid dynamics, and give your thyroid a better chance to function with less medication. The key is personalized dosing, regular monitoring, and collaboration with your healthcare team.
Can I get enough vitamin D from sunlight alone?
In most temperate regions-including Ottawa-winter sunlight provides less than 200 IU per day, which is far below the 1,000‑4,000 IU daily doses needed for thyroid patients. A supplement is usually required year‑round.
Will vitamin D interact with my levothyroxine?
There’s no direct pharmacokinetic interaction, but high calcium from excess vitamin D can impair levothyroxine absorption. Take levothyroxine on an empty stomach and separate it from calcium‑rich meals by at least 30 minutes.
How soon can I expect symptom improvement?
Many patients notice subtle energy gains within 4‑6 weeks, but measurable drops in TPO antibodies usually appear after 3‑6 months of consistent dosing.
Is there a risk of vitamin D toxicity?
Toxicity is rare and typically linked to chronic intake above 10,000 IU/day. Symptoms include nausea, excessive thirst, and high calcium. Regular lab checks keep you safe.
Should I test for vitamin D before starting supplements?
Yes. A baseline 25(OH)D level lets you choose the right loading dose and avoid unnecessary high‑dose supplementation.