When you walk into a doctor’s office and hear your blood pressure reading-say, 138/86-it’s easy to assume you’re in the danger zone. After all, you’ve heard for years that 120/80 is the gold standard. But what if that number isn’t right for you? What if chasing 120/80 means more pills, more side effects, and more trips to the clinic-without actually helping you live longer or feel better?
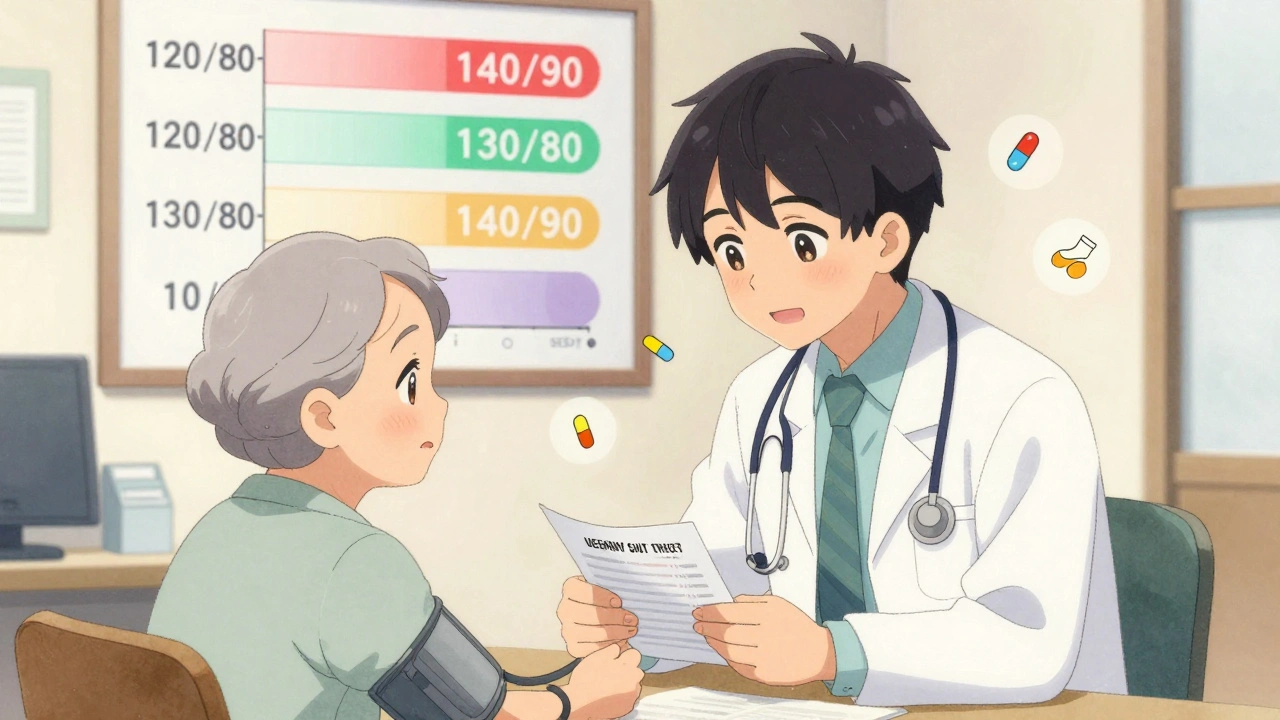
The truth is, there’s no one-size-fits-all number for blood pressure. Major medical groups are split. The American Heart Association and American College of Cardiology say aim for under 130/80, and even push for 120/80 if you can handle it. Meanwhile, the American Academy of Family Physicians says stick with 140/90 for most people. And Japan? They just dropped their old rules and now want everyone under 130/80-no exceptions.
So who’s right? The answer isn’t in the numbers. It’s in the person.
Why 120/80 Got So Popular
The push for lower targets started with the SPRINT trial in 2015. That study followed nearly 9,400 people with high blood pressure but no diabetes or history of stroke. Half were told to get their systolic pressure below 120. The other half aimed for under 140. After about four years, the group with the lower target had 25% fewer heart attacks, strokes, and heart failure episodes. Their death rate dropped by 27%.
That sounded like a miracle. Hospitals, clinics, and apps started pushing 120/80 as the new normal. Media headlines screamed: “Lower Is Better.” Drug companies noticed. The global blood pressure medication market hit $28.7 billion in 2024 and is expected to grow to $33.2 billion by 2027. More targets mean more prescriptions.
But here’s what got left out: the SPRINT participants were carefully selected. They weren’t the typical patient you see in a family doctor’s office. No diabetes. No history of falls. No severe kidney disease. No dementia. And they were closely monitored-every few months-with nurses checking for dizziness, low blood pressure, or kidney changes.
The Other Side: Why 140/90 Still Makes Sense
The American Academy of Family Physicians looked at the same data-and saw something different. They found that while lower targets helped a little, they came with real costs. For every 33 people pushed to hit below 130/80, one would end up with a serious side effect: fainting, kidney trouble, dangerously low blood pressure, or electrolyte imbalances.
That’s not a small number. In the U.S., nearly 122 million adults have high blood pressure. If every one of them were pushed to 120/80, we’d be talking about hundreds of thousands of people with avoidable side effects.
And the extra benefit? Tiny. To prevent one heart attack or stroke, you’d need to treat 137 people for nearly four years just to get one good outcome. That’s a lot of pills, a lot of doctor visits, and a lot of anxiety for a very small gain.
Family doctors see patients who are older, frailer, or juggling multiple conditions. For an 80-year-old with arthritis, memory issues, and three other chronic diseases, dropping their blood pressure to 120 might mean they fall getting out of bed. That’s not health-it’s harm.
What the Experts Actually Recommend
It’s not just AHA vs. AAFP. Europe’s guidelines say: under 129/79 for people under 65, under 139 for those 65 to 79, and under 150 for those 80 and older. Japan says: everyone under 130/80, no matter what. The U.S. guidelines are the most aggressive. The European approach is the most practical. Japan’s is the most uniform.
Here’s what most doctors agree on:
- If your blood pressure is 140/90 or higher, you need treatment-lifestyle changes or meds.
- If you’re under 65 and have diabetes, kidney disease, or a high risk of heart disease, aim for under 130/80.
- If you’re over 75, or have a history of falls, dizziness, or kidney problems, 140/90 is safer and just as effective.
- If you’re in your 50s, healthy, and have no other conditions, going lower than 130/80 might help-but only if you can do it without side effects.
The PREVENT risk calculator, used in 78% of U.S. primary care clinics, helps sort this out. It looks at age, cholesterol, smoking, diabetes, and other factors to predict your 10-year risk of heart disease. If your risk is below 7.5%, you might not need meds at all-just diet, walking, and sleep.
The Real Problem: One Size Doesn’t Fit All
Here’s the uncomfortable truth: guidelines are written for populations, not people. A 62-year-old woman with high blood pressure and a desk job is not the same as a 78-year-old man who walks with a cane and takes five medications for different conditions.
When doctors treat numbers instead of people, things go wrong. A patient gets prescribed a new pill. They feel dizzy. They stop taking it. Their pressure climbs again. They’re labeled “noncompliant.” But the real problem? The treatment didn’t fit their life.
That’s why shared decision-making matters. It’s not a buzzword. It’s the difference between a pill that helps and a pill that hurts.
Ask yourself: Are you feeling better? Are you dizzy when you stand up? Are you falling? Are you on too many pills? Is your blood pressure dropping too low at night? These are the questions that matter more than the number on the screen.
What You Can Do Right Now
You don’t need to wait for a guideline update to take control. Here’s what works:
- Measure your blood pressure at home. Use a validated upper-arm monitor. Write down readings over a week. Bring them to your doctor-not just one number from the clinic.
- Ask: “What’s my 10-year risk of heart disease?” If you don’t know, ask for the PREVENT calculator.
- If you’re on meds, ask: “Is this pill helping me live longer, or just lowering a number?”
- If you’re dizzy, tired, or fainting, tell your doctor. Don’t ignore it. That’s not normal.
- Lifestyle changes still work. Walk 30 minutes a day. Cut added sugar. Sleep 7 hours. These do more than any pill for many people.
The goal isn’t to hit 120/80. The goal is to live longer, feel better, and avoid hospital visits. If you can get to 120/80 without side effects, great. But if you’re struggling, 130/80 or even 140/90 might be the smarter choice.

The Future: Personalized Blood Pressure Care
The next big thing isn’t a new guideline. It’s personalized medicine. Researchers are testing algorithms that combine your genetics, kidney function, sleep patterns, stress levels, and even your neighborhood’s walkability to predict how you’ll respond to different treatments.
The NIH just launched SPRINT-2-a new study with over 8,500 people, including those with diabetes and high fall risk. This time, they’re testing lower targets in the real world, not a controlled trial.
And in Canada, where I live, clinics are starting to use wearable monitors that track blood pressure all day, not just once a month. That’s how we’ll know if your pressure is dropping too low at night-or spiking when you’re stressed.
What’s clear now? Blood pressure isn’t a number. It’s a signal. And the best treatment isn’t the one that lowers it the most. It’s the one that keeps you alive, active, and feeling like yourself.
Is 120/80 the right blood pressure goal for everyone?
No. While 120/80 is often called the ideal, it’s not right for everyone. For healthy adults under 65 with high risk of heart disease, it may be appropriate. But for older adults, those with kidney issues, or people prone to dizziness, aiming for 130/80 or even 140/90 is safer and just as effective at preventing death and disability.
Why do some doctors say 140/90 is fine?
Doctors who recommend 140/90 are often family physicians who treat older, more complex patients. Studies show that pushing people too hard to hit lower targets increases side effects like fainting, kidney problems, and low blood pressure-without significantly improving survival. For many, the risks outweigh the small benefit.
Should I take more pills to get my blood pressure lower?
Not necessarily. Adding more medications increases side effects and cost. If you’re already at 130/80 and feel fine, adding another pill to reach 120/80 might not help you live longer-it might just make you feel worse. Talk to your doctor about whether the trade-off is worth it.
How do I know if my blood pressure treatment is working?
Look beyond the number. Are you sleeping better? Do you feel dizzy when you stand? Are you falling? Can you walk up stairs without getting winded? These matter more than whether your systolic pressure is 125 or 135. If you’re feeling worse, your treatment might be too aggressive.
Can lifestyle changes replace blood pressure meds?
For many people, yes. Losing weight, cutting salt, walking daily, and improving sleep can lower blood pressure as much as a single pill. If you have stage 1 hypertension (130-139/80-89) and low heart disease risk, doctors often recommend trying lifestyle changes for 3-6 months before prescribing meds.
What’s the next big change in blood pressure treatment?
The future is personalization. New tools are being tested that use your genetics, daily activity, sleep patterns, and even where you live to predict how you’ll respond to different treatments. Instead of guessing, doctors will soon know exactly what works for you-without trial and error.
Final Thought: Your Health, Your Choice
High blood pressure is serious. But so are side effects. So is taking too many pills. So is living in fear of a number on a screen.
The best treatment isn’t the one that makes the number look perfect. It’s the one that lets you live your life-without dizziness, without falls, without constant worry.
Ask questions. Track your symptoms. Don’t let a guideline dictate your care. You’re not a statistic. You’re a person-and your goal should be to feel good, not just to hit a number.