When your child gets sick, you want the best care-fast, effective, and safe. That’s why so many parents and doctors turn to generic drugs for kids. They’re cheaper, widely available, and seem like an easy swap for brand-name medications. But here’s the truth: generic drugs for children aren’t always interchangeable, and assuming they are can put your child at risk.
Why Kids Aren’t Just Small Adults
Children’s bodies don’t process medicine the same way adults do. Their liver and kidneys are still developing, their stomachs absorb drugs differently, and their brain chemistry is more sensitive. This isn’t theory-it’s clinical fact. For example, infants under 2 years old produce more glutathione, which makes them less likely to suffer liver damage from acetaminophen than adults. But that same difference means they can’t safely handle certain other drugs. Lamotrigine, used for seizures, carries a much higher risk of life-threatening skin reactions in kids. Verapamil, a heart medication, can cause dangerous drops in blood pressure in newborns. These aren’t edge cases. They’re well-documented risks.That’s why a generic version of a drug that’s perfectly safe for a 40-year-old might be dangerous for a 4-year-old-even if the active ingredient is identical. The FDA requires generics to match brand-name drugs in active ingredients, but nothing says the fillers, dyes, or preservatives have to be the same. And those extra ingredients? They’re often the problem.
The Hidden Dangers in Inactive Ingredients
Think of a pill or liquid medicine like a sandwich. The active ingredient is the meat. The rest-sugars, flavors, alcohol, dyes, preservatives-is the bread and condiments. For adults, it doesn’t matter much. For kids, it can be everything.Benzocaine, a common numbing agent in teething gels and throat sprays, can cause methemoglobinemia-a rare but deadly blood disorder-in children under 2. It’s in some generic versions, not others. Same with propylene glycol, a solvent used in liquid antibiotics. In high doses, it can cause seizures or kidney damage in infants. One study found that 18% of adverse reactions in children linked to generic drugs were caused by these hidden ingredients, not the medicine itself.
Even something as simple as color or taste can cause problems. Parents on Reddit shared stories of kids refusing to take medicine after a switch to a generic version with a different color or flavor. One child developed a rash after switching from brand-name cetirizine to a generic that used a different preservative. Another had severe diarrhea after a switch to generic loperamide. These aren’t rare complaints. In a 2024 survey of over 1,200 parents, 68% reported issues after a generic substitution.
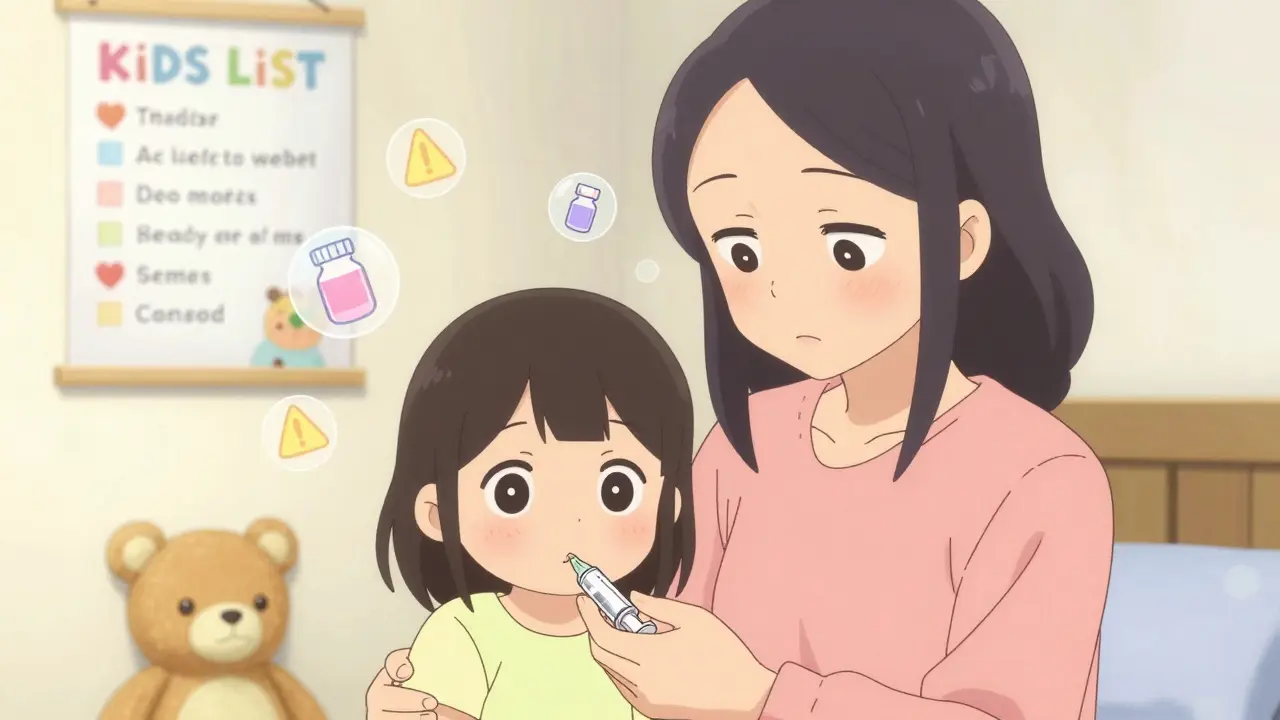
The KIDs List: Your Secret Weapon
There’s a tool most parents don’t know about, but pediatric pharmacists use every day: the KIDs List (Key Potentially Inappropriate Drugs List). It’s maintained by the Pediatric Pharmacy Association and updated quarterly. The list flags 4,149 drugs with known or suspected dangers in children under 18. Each drug is rated by evidence strength and risk level.Some drugs are marked ‘avoid’-meaning the risk of harm outweighs any benefit. Promethazine, a common generic antihistamine, is on that list for kids under 2. It’s been linked to breathing stops and death. Trimethobenzamide, an anti-nausea drug, is also flagged for all patients under 18 because of the risk of sudden, uncontrollable muscle spasms. Even common OTC drugs like guaifenesin (an expectorant) are now listed as ‘avoid’ for children under 4.
Topical drugs are just as risky. Betamethasone creams-used for eczema and diaper rash-come in different strengths. Some generics are labeled ‘very high potency.’ Using those on infants can cause adrenal suppression, Cushing syndrome, or stunted growth. The KIDs List says: don’t use any potent steroid cream on kids under 2 unless a specialist says so.

Off-Label Use: The Silent Epidemic
About 40% of all medications given to children in the U.S. are used in ways not approved by the FDA. That means the label doesn’t say it’s safe or effective for that age, weight, or condition. And 90% of those prescriptions are for generic drugs.Why? Because most drugs were never tested in kids. The FDA didn’t require pediatric studies until the 2000s. Even now, 60% of generic drugs lack specific pediatric dosing info, compared to just 35% of brand-name drugs. So doctors guess. They take the adult dose and scale it down by weight. But that doesn’t always work. A child’s metabolism changes dramatically between ages 1 and 5. A dose that’s perfect at age 3 might be toxic at age 2.
One of the most common errors? Dosing mistakes. A 2023 study found that medication errors in children are three times more common than in adults. Why? Unit confusion-giving 1.0 mL instead of 1 mL, which can mean a tenfold overdose. Or using a household spoon instead of an oral syringe. That’s why the FDA and pediatric experts insist: always use the syringe that comes with the medicine. Never guess.
What You Can Do: A Parent’s Safety Checklist
You don’t need to be a pharmacist to protect your child. Here’s what works:- Ask if the generic is right for your child’s age. Say: “Is this generic version approved for kids under 5?”
- Check the KIDs List. Go to pediatricpharmacy.org and search the drug name. It’s free.
- Read the label. Look for concentration (mg/mL). Never assume a liquid is the same as the last bottle.
- Use an oral syringe. Not a spoon. Not a dropper. A syringe. It’s the only way to get the exact dose.
- Don’t switch brands without talking to your doctor. Even if the name changes, the formula might too.
- Keep a current list. Write down every medicine-prescription, OTC, supplement. Bring it to every appointment.
- Never use adult medicine for a child. Even if it’s “just a little.”

When to Say No to the Generic
Some kids need the brand name. That’s not a luxury-it’s medical necessity. If your child has epilepsy and takes phenytoin, or hypothyroidism and takes levothyroxine, switching generics can cause dangerous fluctuations in blood levels. These drugs have a narrow therapeutic index. That means the difference between a safe dose and a toxic one is tiny.Doctors can write “Dispense as Written” on the prescription. That tells the pharmacy: don’t substitute. You can ask for this. You have the right to ask. If the pharmacist pushes back, ask to speak to the pharmacist on duty. They’re trained to handle these requests.
Some insurance plans try to force generic substitutions. But if your child has had a reaction before, or if the drug is on the KIDs List, you can appeal. Keep a copy of the KIDs List entry. Bring it to your doctor. It’s your best evidence.
The Future Is Changing-But Slowly
There’s progress. In 2024, the FDA required all new generic drug applications to include pediatric dosing information when available. Full compliance is due by December 2025. The European Union is ahead of the U.S.-78% of their pediatric drug applications include safety data. In the U.S., it’s still just 42%.Companies are starting to make better pediatric formulations. More liquids with child-friendly flavors. More tablets that split cleanly. More packaging that prevents accidental overdose. But it’s still a small fraction of the market.
Artificial intelligence is being tested to predict safe doses for kids based on weight, age, and liver function. Early results show 89% accuracy. That’s promising. But until mandatory testing is required for all generics, the burden will stay on parents and doctors to be vigilant.
Bottom Line: Safety Comes First
Generic drugs aren’t bad. They’re essential for keeping healthcare affordable. But for children, they’re not always safe. The assumption that “same active ingredient = same safety” is dangerously wrong.If your child is on a generic drug, ask: Has this been studied for kids? Is it on the KIDs List? Are the inactive ingredients safe for their age? Did we measure the dose correctly?
One wrong dose can change a child’s life. But with the right questions, the right tools, and the right caution-you can keep them safe.