Most people have moles. Some are small, some are dark, and most never change. But when one starts looking different, it’s not just a cosmetic concern-it could be melanoma, the deadliest form of skin cancer. The ABCDE rule was created to help spot warning signs early, and it’s saved lives. But here’s the truth: ABCDE isn’t foolproof. Many melanomas slip through because they don’t fit the textbook picture. Knowing when to trust the rule-and when to ignore it-could mean the difference between catching it early and missing it entirely.
What the ABCDE Rule Actually Means
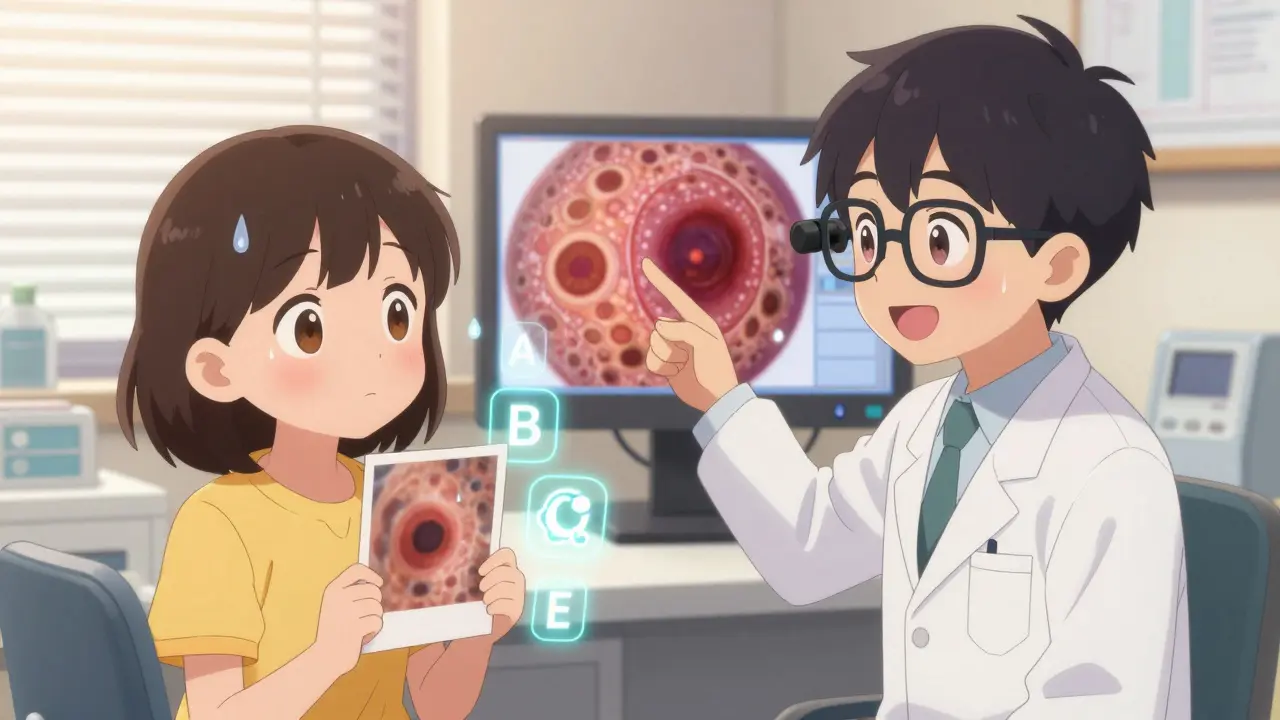
The ABCDE rule breaks down five visual traits to watch for in moles. It’s simple enough for anyone to use during a self-check:- A for Asymmetry: If you draw a line through the middle, both halves don’t match. A normal mole is usually round or oval and balanced. A melanoma looks lopsided, like a smudged ink blot.
- B for Border irregularity: Healthy moles have smooth, even edges. Melanomas often have jagged, notched, or blurred borders that fade into the surrounding skin.
- C for Color variation: A benign mole is usually one shade-light brown, dark brown, or tan. Melanomas show multiple colors: black, red, white, blue, or gray all in the same spot. Even a tiny patch of a new color matters.
- D for Diameter: The old rule said 6 millimeters-about the size of a pencil eraser. But now, experts say 5 millimeters is the new red flag. And here’s the catch: 30% of melanomas are found when they’re smaller than that. So don’t wait for it to get big. If it’s darker than your other moles, even if it’s tiny, pay attention.
- E for Evolving: This is the most important sign. Any change over weeks or months-growing, itching, bleeding, crusting, or changing color-is a major red flag. Melanomas don’t sit still. If a mole you’ve had for years suddenly starts acting weird, get it checked.
Some dermatologists now use ABCDEFG, adding F for Funny looking and G for Growing rapidly. But the core remains ABCDE. The Skin Cancer Foundation says the most reliable warning is change over time. If you’re not sure, take a photo next time you check your skin. Compare it in six months. That’s how most people catch their own melanomas.
Why the ABCDE Rule Misses So Many Melanomas
It’s not just you. The ABCDE rule misses about one in three melanomas-especially early ones. A 2022 study of 144 melanoma cases found that 36% were in situ (stage 0), meaning they hadn’t spread yet. But only 32.7% of those early melanomas showed the classic “E” sign-evolving. That means nearly two-thirds of the most treatable melanomas didn’t look like they were changing.Some melanoma types barely fit the rule at all. Desmoplastic melanoma, for example, often looks like a scar or a rough patch of skin-not a dark mole. Childhood melanomas look different too. In 82% of cases, they didn’t meet ABCDE criteria. And then there’s the “ugly duckling” sign: a mole that looks completely different from all the others on your body. A 2019 study found this sign caught 73% of melanomas that ABCDE missed.
One Reddit user, u/SkinCancerSurvivor, shared: “My melanoma was perfectly symmetrical, uniform color, and only 3mm-none of the ABCDE criteria applied. It was stage IIB.” That’s not rare. In a survey of 1,200 patients by the American Academy of Dermatology, 42% delayed seeing a doctor because their mole didn’t meet enough ABCDE signs. On average, they waited over seven months. That delay can be deadly.
When to Get a Biopsy-It’s Not Just About the Rule
A biopsy is the only way to know for sure if a mole is cancerous. But not every weird-looking mole needs one. Dermatologists use three main triggers:- Three or more ABCDE signs: This has an 85% sensitivity rate-meaning it catches most melanomas. But it also means 28% of biopsies are for harmless moles.
- Documented change over 3-6 months: Even if a mole looks normal, if it’s grown, darkened, or started itching, it’s a biopsy candidate. This criterion is 92% sensitive-more reliable than ABCDE alone.
- The ugly duckling sign: If one mole stands out from the rest, it gets looked at-even if it’s small and symmetrical. Dermatologists are trained to see the whole picture, not just individual moles.
Here’s the problem: most people don’t have baseline photos. The Skin Cancer Foundation says only 19% of patients have pictures of their moles from a year ago. Without that, it’s hard to prove “evolving.” That’s why dermatologists rely on experience. They’ve seen thousands of moles. They know what’s normal for your skin type, your history, your family risk.
And here’s something most people don’t realize: a biopsy isn’t always surgery. Many clinics now use a shave biopsy-just scraping off the top layer. It’s quick, minimally invasive, and often enough to make a diagnosis. Full excision is only needed if the shave result is unclear or shows deeper invasion.
What’s Changing in Melanoma Detection
The ABCDE rule is still the foundation, but it’s no longer the whole story. In 2023, the International Dermoscopy Society launched ABCDE 2.0, which integrates AI tools trained on over 12 million images. These tools analyze patterns invisible to the human eye. The FDA-approved SkinVision app, for example, uses ABCDE plus machine learning and has a 95% sensitivity rate in clinical trials.Dermatologists in 85% of U.S. practices now use digital dermoscopy-a handheld device that magnifies and illuminates the mole. It increases diagnostic accuracy from 75% to 92%. But these tools aren’t for home use. They’re expensive, require training, and aren’t available in most primary care offices.
Even more promising are molecular tests like DecisionDx-Melanoma. This 23-gene test analyzes the genetic profile of a suspicious mole and predicts how likely it is to spread. It’s used in 68% of academic dermatology centers. In a 2022 study, it helped avoid unnecessary surgeries in 31% of cases. That means fewer scars, fewer complications, and less anxiety.
The U.S. Preventive Services Task Force is updating its guidelines as of 2024, moving away from universal screening toward risk-based approaches. That means people with fair skin, a family history, or lots of moles will be prioritized for checks. But for everyone else? The message is clear: don’t wait for the perfect ABCDE checklist. Watch for change.
What You Should Do Right Now
You don’t need a dermatologist to start protecting yourself. Here’s what to do:- Check your skin once a month. Use a mirror, or ask a partner to help with your back, scalp, and between your toes.
- Take a photo of any mole you’re unsure about. Date it. Compare it in six months.
- Don’t wait for all five ABCDE signs. If one thing feels off-especially if it’s changing-get it checked.
- Know your “ugly ducklings.” These are the moles that look different from the rest. They’re often the ones that turn out to be melanoma.
- Don’t ignore a mole just because it’s small. Size isn’t everything. Color change, bleeding, or itching matter more.
- If your doctor says “it’s probably fine,” but you still feel uneasy, ask for a referral to a dermatologist. Your gut feeling matters.
Every year, over 100,000 new melanomas are diagnosed in the U.S. alone. And every year, thousands are caught too late-not because people ignored warning signs, but because they were looking for the wrong ones. The ABCDE rule is a tool, not a rulebook. It’s a starting point. The real goal is to notice anything unusual and act before it spreads.
What Happens After a Biopsy
If your mole is removed, the pathologist will examine it under a microscope. Results usually come back in 7-10 days. If it’s melanoma, they’ll report the depth (Breslow thickness), whether it’s ulcerated, and if cancer cells are at the edges of the sample. That determines your next steps.Stage 0 (in situ) melanoma means the cancer is only in the top layer of skin. Surgery to remove a small margin around it is usually all that’s needed. The five-year survival rate is 99%.
If it’s deeper, you may need a wider excision, a sentinel lymph node biopsy, or even immunotherapy. But early detection is the key. That’s why even a tiny, weird-looking mole deserves a look.
Can a mole be cancerous even if it doesn’t fit the ABCDE rule?
Yes. About 20-30% of melanomas don’t show classic ABCDE signs. Some are perfectly symmetrical, uniform in color, and smaller than 5mm. The most important sign is change-any mole that’s evolving, bleeding, itching, or looking different from your other moles should be checked, even if it doesn’t match the rule.
Is it safe to wait and watch a suspicious mole instead of removing it right away?
No. Waiting to see if a mole changes is risky. Melanoma can grow quickly-sometimes in weeks. If you notice a change, get it evaluated immediately. Dermatologists use tools like dermoscopy and digital imaging to monitor moles safely without rushing to surgery. But if there’s any doubt, a biopsy is the only way to be sure.
Do I need to get every new mole checked?
Not every new mole is dangerous. Most moles appear in childhood and adolescence. New moles after age 35 are more likely to be suspicious, especially if they’re dark, irregular, or growing. But any new spot that looks different from your other moles-especially if it’s dark, changing, or bleeding-should be checked. Don’t assume it’s harmless just because it’s new.
Can I rely on apps or AI tools to check my moles at home?
Apps like SkinVision can help you track changes and flag potential concerns, but they’re not a replacement for a dermatologist. These tools have high sensitivity, but they can still miss melanomas or flag harmless moles as suspicious. Use them as a reminder to see a professional-not as a diagnosis.
How often should I get a professional skin check?
If you have no risk factors (fair skin, family history, many moles), an annual check is fine. If you’ve had melanoma before, have more than 50 moles, or have a family history, you should be checked every 6 months. People with a history of sunburns or tanning bed use should also get checked more often. Monthly self-checks are essential no matter your risk level.







