What Is a Pulmonary Embolism?
A pulmonary embolism (PE) happens when a blood clot blocks one or more arteries in your lungs. These clots usually start in the deep veins of your legs - a condition called deep vein thrombosis (DVT) - and travel upward until they get stuck in your lungs. Once there, they stop blood from flowing properly, which means your lungs can’t get enough oxygen to your body. This isn’t just a minor issue. It’s a medical emergency that kills about 100,000 people in the U.S. every year.
The scary part? Many people don’t realize what’s happening until it’s too late. The most common symptom - sudden shortness of breath - is often mistaken for anxiety, asthma, or just being out of shape. In fact, 85% of people with PE report this symptom. But unlike typical breathlessness from exercise, this comes out of nowhere, even when you’re sitting still. Some describe it like trying to breathe through a straw while running.
Sudden Shortness of Breath: The Biggest Red Flag
If you suddenly can’t catch your breath - especially if it’s worse than normal and doesn’t improve with rest - it’s not something to ignore. This isn’t just feeling winded after climbing stairs. This is the kind of breathlessness that makes you stop mid-sentence, clutch your chest, and wonder if you’re having a heart attack.
Studies show that 92% of people with a massive PE (a clot blocking a major artery) have severe shortness of breath even at rest. For others with smaller clots, the breathlessness might be mild at first, then get worse over days. That’s why so many people delay going to the doctor. One patient on a lung health forum said she thought her breathlessness was anxiety for three weeks before she collapsed. She was diagnosed with PE the same day.
Other symptoms often show up alongside it:
- Chest pain that gets worse when you breathe in or cough (74% of cases)
- A dry cough or coughing up blood (23% have hemoptysis)
- Swelling, warmth, or pain in one leg (44% have DVT)
- Rapid heartbeat (over 100 bpm in 30% of cases)
- Feeling lightheaded or fainting (14% of cases)
None of these are unique to PE. That’s why it’s so easy to miss. But when you combine sudden breathlessness with leg swelling or unexplained rapid heartbeat, the risk goes up fast.
Why Diagnosis Is So Often Delayed
Emergency rooms see thousands of people with shortness of breath every day. Most have asthma, pneumonia, or heart failure. PE is rare compared to those. So doctors start by ruling out the common stuff.
But here’s the problem: PE doesn’t always show up on a chest X-ray. In fact, 80% of PE patients have a normal X-ray. Blood tests might look fine too. That’s why many people get sent home with a diagnosis of bronchitis or anxiety - only to come back worse days later.
A 2022 survey of 1,200 PE patients found that 68% visited a doctor at least twice before getting the right diagnosis. One in four was initially told they had pneumonia or asthma. One Reddit user wrote: “I went in with sharp chest pain and shortness of breath. They gave me an inhaler. I passed out two days later. That’s when they found the clot.”
Delays aren’t just frustrating - they’re deadly. Every hour counts. The longer a clot stays, the more damage it does to your lungs and heart. And if it’s large enough, it can cause sudden cardiac arrest.
How Doctors Diagnose Pulmonary Embolism
There’s no single test that catches every PE. Doctors use a step-by-step approach to avoid missing it - and avoid over-testing healthy people.
The first step is figuring out your risk. Doctors use tools like the Wells Criteria or the Geneva Score. These are simple checklists that ask questions like:
- Do you have recent surgery or immobilization?
- Do you have a history of DVT or PE?
- Is your heart rate over 100?
- Do you have leg swelling?
Based on your answers, you’re labeled low, moderate, or high risk. This tells the doctor how likely it is you have PE - and what to do next.
The Role of the D-Dimer Test
If you’re low risk, doctors often start with a D-dimer test. This blood test looks for fragments of broken-down clots. If the result is normal, and you’re low risk, PE is almost certainly ruled out - with 97% accuracy.
But here’s the catch: D-dimer goes up with age, pregnancy, infection, cancer, or even recent surgery. So for people over 50, the test isn’t reliable on its own. That’s why doctors now use age-adjusted D-dimer thresholds. For someone 70 years old, a result under 700 ng/mL might be considered normal - not the old standard of 500.
And if you have cancer? Your D-dimer is often high even without a clot. In that case, doctors skip the test and go straight to imaging.
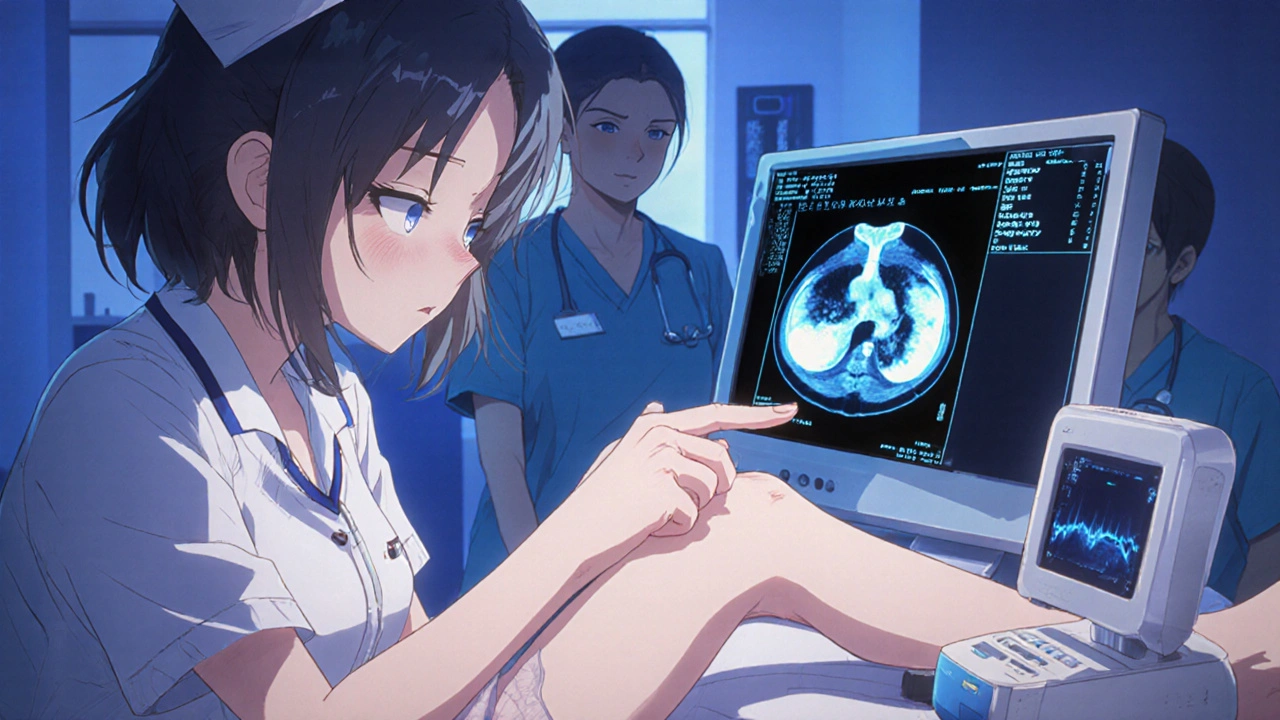
CTPA: The Gold Standard for Confirmation
If your risk is moderate or high, or your D-dimer is elevated, the next step is a CT pulmonary angiogram (CTPA). This is a special CT scan that uses contrast dye to show the blood vessels in your lungs. It’s accurate in 95% of cases and can show exactly where the clot is.
It’s not perfect. You need to be able to tolerate contrast dye, and there’s a small amount of radiation. But it’s fast - most hospitals can do it within an hour. And it’s the best way to confirm PE and rule out other problems like pneumonia or a collapsed lung.
For people who can’t have contrast - like those with kidney disease or allergies - doctors use a V/Q scan. This test looks at airflow and blood flow in the lungs. It’s less common because not every hospital has the equipment, but it’s just as accurate when done right.
Ultrasound for the Clot’s Origin
Since most clots start in the legs, doctors often check for DVT with a compression ultrasound. It’s painless, no radiation, and takes about 15 minutes. If they find a clot in your leg, and you have symptoms like shortness of breath, they can treat you for PE without even doing a CTPA.
This is especially helpful in emergency rooms where time matters. If you have leg swelling and sudden breathlessness, and the ultrasound shows a clot, you’re treated as if you have PE - because the risk is too high to wait.
What Happens If You’re Unstable?
If you’re in shock - low blood pressure, passing out, turning blue - doctors don’t wait for scans. They go straight to a bedside echocardiogram (ultrasound of the heart). If they see right ventricular strain - meaning your heart is struggling to pump against the clot - they know you have a massive PE and need immediate treatment.
This isn’t just about diagnosis. It’s about saving your life. People with massive PE who get treated within 60 minutes have a much better chance of survival.

Why Early Detection Saves Lives
Thanks to better protocols, PE mortality has dropped from 8.5% in 2015 to 5.2% in 2022. Hospitals that use structured pathways - like checking risk, ordering D-dimer, and doing CTPA within 90 minutes - cut death rates in half.
One hospital in Ontario reduced time-to-diagnosis from over two hours to under 45 minutes. Their PE-related deaths fell from 8.2% to 3.1% in a year.
It’s not just about technology. It’s about training. Emergency staff who get four hours of training on the Wells Criteria are 85% more consistent in spotting high-risk patients.
Who’s at Highest Risk?
Some people are at much higher risk:
- People who’ve had a previous PE or DVT (33% have another within 10 years)
- Cancer patients (4.7 times more likely to get PE)
- Those who’ve had recent surgery or trauma
- People on birth control or hormone therapy
- Those who’ve been immobilized for long periods (hospital stays, long flights)
- People over 60
If you fall into one of these groups and get sudden breathlessness, don’t wait. Don’t assume it’s stress or aging. Go to the ER.
What Comes After Diagnosis?
If you’re diagnosed with PE, you’ll start blood thinners right away - usually injectable or oral anticoagulants. Most people go home after a few days, but those with massive clots or heart strain may need intensive care.
Long-term, you’ll likely take blood thinners for at least three months. Some need them for life, especially if they have cancer or repeated clots.
Follow-up is key. You’ll need ultrasounds to check if the leg clot is gone, and your doctor will monitor for side effects like bleeding. And if you’ve had one PE, you’re at higher risk for another - so watch for symptoms again.
What You Can Do Now
You can’t always prevent a clot, but you can reduce your risk:
- Move regularly - don’t sit for hours without stretching
- Stay hydrated, especially on long flights
- Wear compression socks if you’re at risk
- Talk to your doctor about blood thinners if you’ve had a prior clot
- Know your symptoms - and act fast
If you ever get sudden shortness of breath - especially with leg swelling, chest pain, or a racing heart - don’t wait. Call 911 or go to the nearest emergency room. Your life could depend on it.
Can you have a pulmonary embolism without knowing it?
Yes, but it’s rare. Small clots in the outer edges of the lungs may cause mild, temporary breathlessness that fades without treatment. But even these can grow or break off again. Most people who have PE notice symptoms - even if they’re mild at first. The danger is when symptoms are dismissed as something else, like anxiety or a cold. That’s when it becomes life-threatening.
Is a pulmonary embolism the same as a heart attack?
No. A heart attack happens when blood flow to the heart muscle is blocked, usually by a clot in a coronary artery. A pulmonary embolism is a clot in the lungs’ arteries. They can both cause chest pain and shortness of breath, but the causes and treatments are different. A heart attack affects the heart; PE affects the lungs and puts extra strain on the heart. Both are emergencies, but they require different tests and treatments.
Can a blood test alone diagnose a pulmonary embolism?
No. The D-dimer test can help rule out PE if it’s negative and you’re low risk, but it can’t confirm it. Many conditions - infection, surgery, pregnancy, cancer - raise D-dimer levels. A positive result doesn’t mean you have a clot. Only imaging like CTPA or V/Q scan can confirm PE. That’s why doctors use a combination of risk assessment, blood tests, and scans.
How long does it take to recover from a pulmonary embolism?
Recovery varies. Most people feel better within weeks after starting blood thinners, but full recovery can take months. Fatigue and breathlessness linger in about 30% of patients for up to a year. If the clot was large and damaged the lungs or heart, long-term issues like pulmonary hypertension can develop. Regular follow-ups and rehab programs help improve outcomes.
Are there new tests for pulmonary embolism coming soon?
Yes. Researchers are testing new blood biomarkers - like soluble thrombomodulin and plasmin-antiplasmin - that could help detect clots earlier and more accurately than D-dimer. AI tools are also being used to analyze CT scans faster and with fewer missed diagnoses. One AI algorithm recently showed 96% accuracy in detecting PE. These tools aren’t widely used yet, but they’re expected to become standard in the next few years, especially in large hospitals.