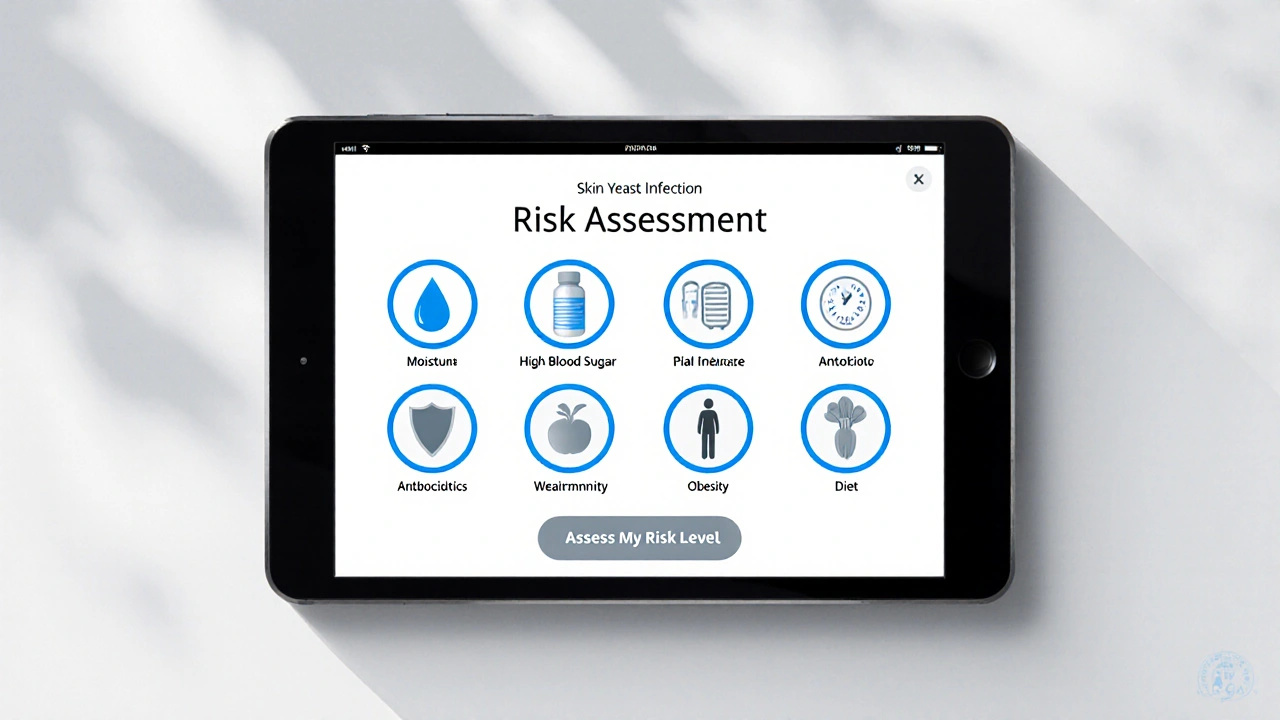
Skin Yeast Infection Risk Assessment
This assessment helps identify potential risk factors for skin yeast infections. Click on each factor that applies to you to see personalized prevention recommendations.
Select Your Risk Factors
Sweaty clothing, prolonged dampness, or occlusive dressings
Diabetes or a carbohydrate-heavy diet
Broad-spectrum antibiotics that disrupt beneficial bacteria
Conditions like HIV, chemotherapy, or chronic steroid use
Extra skin folds that collect moisture
High sugar intake and lack of probiotics
Your Personalized Prevention Plan
Select your risk factors and click "Assess My Risk Level" to receive personalized prevention tips.
When it comes to cutaneous candidiasis is a yeast infection of the skin caused primarily by Candida albicans, most people think of it as a rare problem that only shows up in hospitals. The truth is far from that - everyday habits, climate, and even the food you eat can create the perfect breeding ground for this stubborn fungus. If you’ve ever wondered why a rash keeps popping up in warm folds or why a friend keeps battling “yeast rash” after a course of antibiotics, you’re not alone. Below you’ll find the exact steps you can take today to prevent yeast infections of the skin and keep the irritation at bay.
Key Takeaways
- Yeast infections thrive in warm, moist environments - control humidity on your skin.
- Balanced blood sugar and a healthy immune system are major defenses.
- Simple changes in clothing, hygiene, and diet can cut the risk dramatically.
- Know the early signs and when to call a dermatologist.
What Exactly Is a Skin Yeast Infection?
A skin yeast infection, medically known as cutaneous candidiasis, occurs when the fungus Candida albicans multiplies on the surface of the skin. While Candida lives harmlessly on most people as part of the skin microbiome, certain conditions tip the balance from friend to foe. Typical manifestations include red, itchy patches, sometimes with a satellite rash just outside the main area. Common hotspots are skin folds (under the breasts, groin, armpits), between toes, and anywhere dampness lingers.
Why Some People Get It More Often
Understanding the risk factors helps you target prevention where it matters most. The biggest culprits are:
- Moisture retention: Sweaty clothing, prolonged dampness, and occlusive dressings create a breeding ground.
- High blood sugar: Diabetes or a carbohydrate‑heavy diet fuels yeast growth.
- Antibiotic use: Broad‑spectrum antibiotics knock out beneficial bacteria, giving Candida a free pass.
- Weakened immunity: Conditions like HIV, chemotherapy, or chronic steroid use reduce the body’s ability to keep fungi in check.
- Obesity: Extra skin folds mean more places for moisture to collect.
Even if you don’t fall into any of these categories, everyday habits can still tip the scale. That’s why a preventive routine matters for everyone.
Day‑to‑Day Prevention Checklist
Think of this as your skin‑friendly cheat sheet. Tick each box daily or weekly to keep Candida at bay.
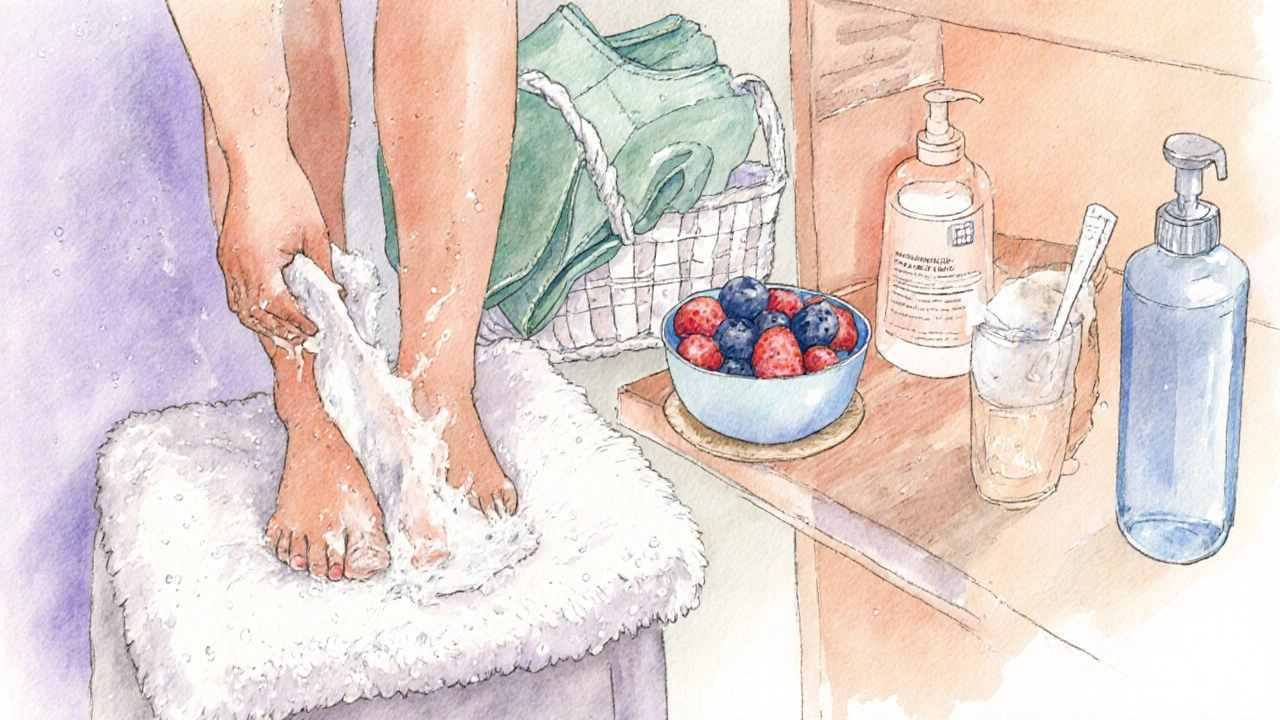
- Keep skin dry: After showering, pat-not rub-wet areas dry. Use a soft towel for skin folds.
- Choose breathable fabrics: Cotton, moisture‑wicking athletic wear, and loose‑fitting clothes let air circulate.
- Change after sweating: Whether it’s a workout or a hot day, swap out damp shirts, socks, and underwear within an hour.
- Mind your diet: Limit sugary snacks and refined carbs. Include probiotic‑rich foods like yogurt, kefir, and sauerkraut to support healthy bacteria.
- Control blood sugar: For diabetics, maintain target glucose levels; even modest spikes can encourage fungal growth.
- Use gentle cleansers: Harsh soaps strip the skin’s natural oils, disrupting the microbiome. Opt for fragrance‑free, pH‑balanced cleansers.
- Apply barrier creams: In areas prone to friction (inner thighs, under breasts), a thin layer of zinc‑oxide or petroleum‑based ointment creates a moisture barrier.
- Limit antibiotic exposure: Only take them when prescribed, and finish the full course. Talk to your doctor about probiotic supplements if you need long‑term antibiotics.
- Stay active, stay clean: Regular exercise improves circulation, but always shower promptly and change clothes afterward.
- Check skin regularly: Early signs-small red bumps, itching, or a shiny sheen-are easier to treat than a full‑blown rash.
Clothing Choices That Make a Difference
What you wear can be a hidden trigger. Here’s how to pick smarter:
- Underwear: Seamless, cotton briefs or boxer briefs; avoid synthetic blends that trap heat.
- Socks: Choose moisture‑wicking athletic socks; change them if they get damp.
- Sports gear: Look for breathable, antimicrobial fabrics. Many brands now embed silver ions that curb fungal growth.
- Footwear: Open‑toed shoes or sandals let feet breathe. If you need closed shoes, rotate pairs and let them air out overnight.
When Lifestyle Isn’t Enough: Spotting Early Infection
Even with perfect habits, a yeast infection can sneak in. Catch it early with these visual cues:
| Symptom | Typical Location | What It Looks Like |
|---|---|---|
| Itching | Any skin fold | Persistent urge to scratch, especially after sweating |
| Redness | Groin, under breasts, between toes | Bright red patches that may spread outward |
| Satellite lesions | Near main rash | Smaller red bumps surrounding a larger patch |
| Moist or “wet” feeling | Skin folds | Skin feels glossy, sometimes with a foul odor |
If you notice any of these, apply an OTC topical antifungal (e.g., clotrimazole 1% cream) for a week and see if it improves. No change? Time to call a dermatologist.
Medical Options: From Topical Creams to Systemic Therapy
While the focus here is prevention, it helps to know what treatment looks like should a breakout occur.
- Topical antifungals: Clotrimazole, miconazole, and terbinafine are first‑line. Apply twice daily for 7‑14 days.
- Oral antifungals: Fluconazole or itraconazole are reserved for extensive or recurrent cases.
- Barrier ointments: Zinc oxide or dimethicone can soothe irritated skin while preventing moisture buildup.
- Probiotic supplementation: Strains like Lactobacillus rhamnosus may rebalance the skin microbiome over weeks.
Doctors often combine lifestyle tweaks with medication for the fastest relief.
Do’s vs. Don’ts: A Quick Reference Table
| Do | Don’t |
|---|---|
| Wear breathable, cotton clothing | Stay in tight, non‑breathing fabrics for long periods |
| Dry skin folds thoroughly after bathing | Leave moisture to sit in creases |
| Change out of sweaty clothes promptly | Reuse damp socks or underwear |
| Limit added sugars and refined carbs | Consume large amounts of sugary drinks and snacks |
| Take probiotics during or after antibiotic courses | Skip probiotic support after antibiotics |

Special Situations: Pregnancy, Diabetes, and the Elderly
Each of these groups faces unique challenges.
- Pregnancy: Hormonal shifts increase moisture in skin folds. Stick to cotton underwear and use gentle, pregnancy‑safe antifungal creams if needed.
- Diabetes: Keep glucose levels stable; regular foot checks are vital because peripheral neuropathy can mask early itching.
- Elderly: Skin thins with age, making it more prone to irritation. Gentle cleansers and daily moisture‑locking lotions help maintain barrier function.
Putting It All Together: A Sample Weekly Routine
Here’s a realistic schedule you can copy‑paste into your phone notes.
- Morning shower: Use a fragrance‑free cleanser; pat dry, especially in groin and under breasts.
- Apply a thin layer of barrier cream to any folds.
- Dress in cotton underwear and breathable socks.
- Breakfast: Include probiotic yogurt and a handful of berries (low sugar).
- Midday: If you’ve sweated, change tops and re‑dry any wet areas.
- Evening: Light stretch or walk, then shower again; repeat drying routine.
- Before bed: Inspect skin for redness or itching; if anything looks off, treat with OTC cream.
Consistency beats occasional mega‑clean‑ups every time.
Frequently Asked Questions
Can diet alone prevent skin yeast infections?
Diet is a strong piece of the puzzle but not a solo solution. Reducing sugar helps keep Candida in check, while probiotic foods support the good bacteria that compete with yeast. Pairing dietary changes with good hygiene and breathable clothing gives the best odds of staying clear.
Are OTC creams safe for long‑term use?
Most over‑the‑counter antifungals are safe for a 2‑week course. Using them repeatedly without a break can irritate skin, so if you need them more than twice a year, see a dermatologist to explore underlying causes and possibly a prescription regimen.
Why do I get rashes under my breasts even though I keep them clean?
Moisture is often the hidden enemy. Even after cleaning, sweat or trapped moisture from bras can create a humid micro‑environment. Switch to moisture‑wicking bras, apply a thin barrier ointment, and make sure the area dries completely before dressing.
Can I use natural remedies like tea tree oil?
Tea tree oil has antifungal properties, but it can also irritate sensitive skin if not diluted. A 5% dilution in a carrier oil is a common recommendation, but start with a patch test. For persistent infections, stick with clinically proven antifungals.
My child keeps getting diaper rash-how can I stop it?
Frequent diaper changes are key. Use a breathable diaper cloth or a super‑absorbent brand that wicks moisture away. After each change, let the skin air‑dry for a minute, then apply a zinc‑oxide diaper rash cream as a barrier.
Next Steps If You Still Have Questions
Even with the best routine, occasional flare‑ups happen. Keep a short log of when symptoms appear, what you ate, and any recent medications. Share that with a dermatologist-they’ll spot patterns you might miss and can tailor a prevention plan just for you. Remember, preventing skin yeast infections isn’t about a single miracle move; it’s about a series of small, consistent habits that keep Candida in its place.