When plaque builds up in the neck arteries, the risk of a disabling stroke spikes dramatically. Doctors often reach for antiplatelet drugs to keep blood clots at bay, but not every pill works the same way. Below we unpack the role of clopidogrel in treating carotid artery disease, why it matters, and how it stacks up against other options.
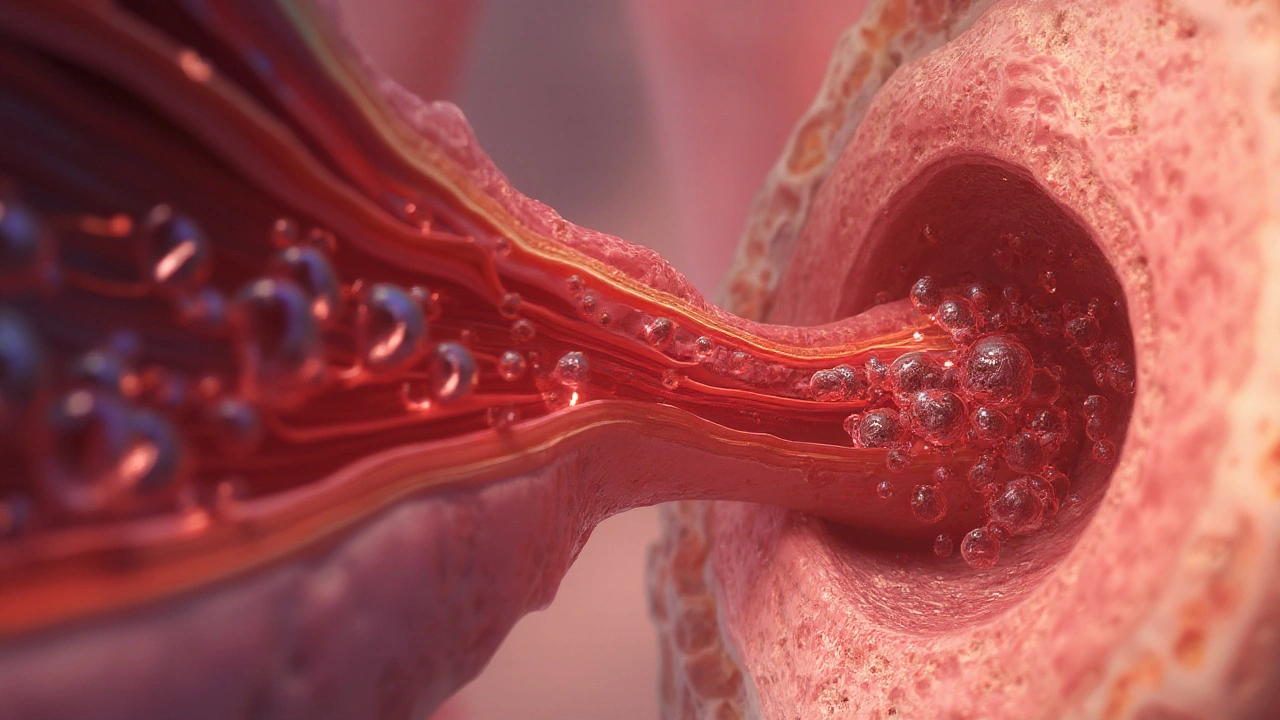
Understanding Carotid Artery Disease
Carotid artery disease is a narrowing of the major arteries that supply blood to the brain, typically caused by atherosclerotic plaque. The condition can be silent for years, yet even a modest blockage (50‑70%) can trigger a transient ischemic attack (TIA) or a full‑blown stroke if a clot dislodges. Risk factors include high LDL cholesterol, hypertension, smoking, and diabetes. Diagnosis usually starts with a duplex ultrasound a non‑invasive imaging test that visualizes blood flow and measures plaque thickness. When the stenosis exceeds 70% or the patient has symptoms, physicians consider surgical (carotid endarterectomy) or endovascular (stenting) interventions, often alongside medication.
What Is Clopidogrel?
Clopidogrel is a thienopyridine‑class antiplatelet agent that irreversibly inhibits the P2Y12 receptor on platelets, preventing aggregation. Commercially known as Plavix, it was approved by the FDA in 1997 and quickly became a staple for secondary prevention after myocardial infarction and peripheral artery disease. Its pharmacokinetic profile features a pro‑drug that requires hepatic conversion via CYP2C19; genetic variations in this enzyme can affect drug efficacy, a fact clinicians now factor into prescribing decisions.
How Clopidogrel Helps Carotid Patients
The primary threat in carotid disease is a platelet‑rich thrombus forming on ulcerated plaque. By blocking ADP‑mediated platelet activation, clopidogrel reduces the likelihood of clot formation without significantly raising bleeding risk compared to more potent agents. Studies show that patients on clopidogrel plus aspirin (dual antiplatelet therapy, DAPT) have a 30‑40% lower incidence of peri‑procedural stroke after carotid stenting than those on aspirin alone.
Clinical Evidence: Trials and Real‑World Data
The landmark CAPRIE trial (Clopidogrel vs. Aspirin) enrolled over 19,000 patients with atherosclerotic disease, including a sizable carotid subgroup. Results revealed a 8.7% relative risk reduction for ischemic events in the clopidogrel arm. More recent registries, such as the CREST trial’s medical‑therapy arm, confirmed that clopidogrel‑based regimens match aspirin in long‑term stroke prevention but offer better protection in patients with high‑risk plaque characteristics (e.g., echolucent cores on ultrasound).
Comparing Antiplatelet Options
Several drugs vie for the antiplatelet spotlight. Below is a side‑by‑side look at the three most used agents for carotid disease.
| Agent | Mechanism | Key Trial | Bleeding Risk | Typical Dose |
|---|---|---|---|---|
| Clopidogrel | P2Y12 receptor inhibition (irreversible) | CAPRIE | Low‑moderate | 75 mg daily |
| Aspirin | COX‑1 inhibition, reduces thromboxane A2 | ASA‑Carotid | Moderate (gastrointestinal) | 81-325 mg daily |
| Ticagrelor | P2Y12 reversible inhibition | SOCRATES (stroke cohort) | Higher (dyspnea, bleeding) | 90 mg BID |
In practice, clopidogrel shines when patients cannot tolerate high‑dose aspirin or when genetic testing shows reduced CYP2C19 activity, making the drug a better alternative to aspirin alone. Ticagrelor offers faster platelet inhibition but at the cost of more side‑effects, so it’s generally reserved for high‑risk acute coronary scenarios rather than chronic carotid management.
Integrating Clopidogrel Into a Treatment Plan
When a physician decides on clopidogrel, the typical regimen starts after confirming the patient’s CYP2C19 genotype (if available) and ensuring adequate renal function. The steps usually look like this:
- Order a genetic test for CYP2C19 metabolizer status.
- Begin 75mg of clopidogrel daily, preferably with a low‑dose aspirin (81mg) if the patient has undergone recent stenting.
- Schedule a follow‑up duplex ultrasound at 3‑6 months to assess plaque stability.
- Monitor for bruising, GI upset, or new neurologic symptoms; adjust dose or switch agents if bleeding becomes problematic.
- Re‑evaluate the need for long‑term DAPT after one year; many guidelines recommend switching to single‑agent therapy thereafter.
Patients also need to control modifiable risk factors: statins for LDL‑C reduction, antihypertensives, smoking cessation, and regular exercise. Combining clopidogrel with high‑intensity statins (e.g., rosuvastatin 20mg) provides a synergistic effect on plaque regression, as shown in the IMPROVE‑IT trial’s subgroup analyses.
Potential Pitfalls and How to Avoid Them
- Drug interactions: Proton‑pump inhibitors like omeprazole can blunt clopidogrel activation; using pantoprazole is a safer alternative.
- Bleeding concerns: Elderly patients (≥80years) have a higher baseline bleed risk; dose adjustment or switching to aspirin may be warranted.
- Non‑adherence: Missing doses reduces platelet inhibition dramatically. Simple reminder apps or blister packs improve compliance.
- Genetic non‑responders: Approximately 30% of East Asian patients carry loss‑of‑function alleles; for them, ticagrelor or prasugrel may be more effective.
Related Concepts and Next Steps
Understanding clopidogrel’s place involves a web of interconnected topics. Here are a few you’ll likely explore next:
- Platelet function testing - lab methods (VerifyNow, PFA‑100) to quantify drug effect.
- Carotid endarterectomy - surgical removal of plaque, often recommended when stenosis >70%.
- Carotid stenting - a less invasive alternative that usually requires short‑term DAPT.
- Transient ischemic attack (TIA) - a warning sign that prompts immediate vascular assessment.
- Stroke secondary prevention - a broader strategy that includes blood pressure control, anticoagulation for atrial fibrillation, and lifestyle changes.
Each of these topics deepens the conversation about how to keep the brain’s blood supply safe and reliable.

Frequently Asked Questions
Can clopidogrel be used alone for carotid artery disease?
Yes, clopidogrel monotherapy is an option, especially for patients who cannot tolerate aspirin. However, many clinicians prefer a short course of dual antiplatelet therapy (clopidogrel+low‑dose aspirin) after carotid stenting to lower early‑trial stroke risk.
How long should I stay on clopidogrel?
Guidelines suggest 1‑12months depending on the intervention. For medical management without a recent procedure, lifelong low‑dose clopidogrel (or aspirin) is often recommended to keep plaque from triggering a clot.
What are the signs of a bleed while on clopidogrel?
Unexplained bruising, black stools, persistent nosebleeds, or gum bleeding should prompt a call to the doctor. In rare cases, intracranial hemorrhage can occur, so any sudden severe headache or neurological change needs urgent evaluation.
Do I need regular blood tests while taking clopidogrel?
Routine platelet counts are not required for most patients, but a baseline CBC is useful. If you’re also on anticoagulants or have kidney disease, your physician may monitor more closely.
Is clopidogrel safe for people with a history of stomach ulcers?
Clopidogrel carries a lower gastrointestinal bleeding risk than high‑dose aspirin, but it’s still prudent to use a proton‑pump inhibitor (preferably pantoprazole) and avoid NSAIDs.