If you live with irritable bowel syndrome, you’ve probably tried everything: bland diets, probiotics, stress management, prescription meds that made you drowsy or constipated. And now you’re wondering if peppermint oil is just another trendy remedy-or if it actually works. The answer isn’t simple, but the science is clearer than you might think.
Why Peppermint Oil Works for IBS
Peppermint oil isn’t just for fresh breath or minty desserts. Its real power comes from L-menthol, the main compound in the oil. This isn’t just a flavor-it’s a muscle relaxant that targets the smooth muscles lining your intestines. When you take enteric-coated peppermint oil, L-menthol blocks calcium channels in those muscles, reducing painful spasms and cramping. It also activates TRPM8 receptors, which help calm the nervous system’s overreaction to normal gut movements-a big part of why IBS feels so unpredictable.The Evidence: It’s Not Just Anecdotal
A 2014 meta-analysis published in the Journal of Clinical Gastroenterology looked at five high-quality studies involving nearly 400 people with IBS. Those who took enteric-coated peppermint oil were more than twice as likely to report overall symptom improvement compared to those on placebo. That’s not a small effect-it’s comparable to some prescription antispasmodics. The European Medicines Agency officially approved peppermint oil for IBS in 2014. The American College of Gastroenterology followed in 2022, giving it a conditional first-line recommendation based on moderate-quality evidence. That’s rare for a herbal remedy. Twelve randomized trials involving over 800 patients have shown consistent results: peppermint oil reduces abdominal pain, bloating, and discomfort better than sugar pills. But here’s the catch: not all peppermint oil is the same. If you swallow a regular capsule or drop oil on your tongue, it dissolves in your stomach. That causes heartburn, nausea, and even worsens symptoms. That’s why only enteric-coated capsules work. These are designed to pass through the stomach and release the oil in the small intestine, where it’s needed.How to Take It: Timing, Dose, and Form
The standard dose is 0.2 to 0.4 mL of peppermint oil-usually delivered in 180-200 mg enteric-coated capsules-taken three times a day, about 30 minutes before meals. Taking it with food reduces effectiveness. Taking it too late after eating? You might miss the window when your gut needs calming. Two popular branded options are IBgard® and Colpermin®. IBgard® uses a triple-coated microsphere system that targets the small intestine more precisely. In one study, users saw a 40% drop in total IBS symptoms-nearly double the placebo effect. Generic enteric-coated capsules can work too, but quality varies. Look for the USP Verified Mark. Independent tests found only 62% of commercial products meet basic purity standards. Start low. Some people get mild heartburn at first. Mayo Clinic doctors suggest starting with one capsule daily for a week, then increasing to three if tolerated. About 28% of new users experience temporary discomfort that fades within days.Who It Works Best For (and Who Should Skip It)
Peppermint oil shines for people with IBS-C (constipation-predominant) and IBS-M (mixed). Studies show 68% of these users report meaningful improvement. But if you have IBS-D (diarrhea-predominant), it might make things worse. The oil’s relaxing effect on the gut can speed up transit time too much, leading to looser stools. It’s also not for everyone. If you have GERD or a hiatal hernia, peppermint oil can relax the lower esophageal sphincter and trigger acid reflux. Pregnant women should avoid it unless cleared by a doctor. And don’t use it if you’re already on proton pump inhibitors (PPIs)-they change stomach pH and can stop the enteric coating from working properly. One study showed this cuts effectiveness by 37%.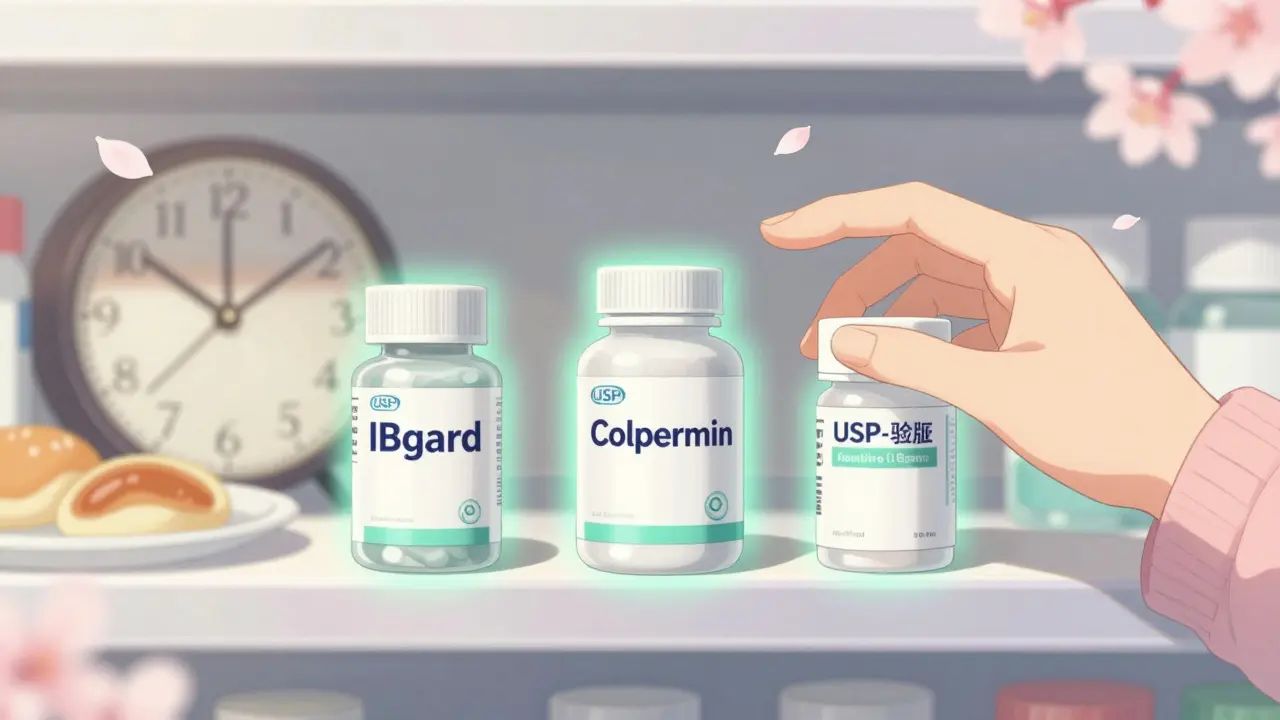
How It Compares to Other Treatments
Let’s say you’re weighing options. Here’s how peppermint oil stacks up:- vs. Placebo: 2.23 times more likely to improve symptoms
- vs. Hyoscine butylbromide (Buscopan): Just as effective
- vs. Trimebutine: Less effective
- vs. Loperamide (Imodium): Better for pain, not diarrhea
- vs. Eluxadoline (Viberzi): Less effective, but far cheaper and with fewer side effects
Real People, Real Results
On Drugs.com, 62% of 247 users rated peppermint oil positively. Common comments: “Cramps gone in 20 minutes,” “Finally stopped the bloating that ruined my workdays,” and “I quit three prescriptions after this worked.” But negative reviews are loud too. “Heartburn worse than my IBS,” “Works one day, useless the next,” and “Wasted $50.” The difference? Timing and quality. A 2021 patient-led study found 84% of users who took capsules 20-30 minutes before meals saw results. Only 52% did when they took them with food. And 42% of negative reviews came from people using non-enteric-coated products.What Experts Say
Dr. William Chey from the University of Michigan calls peppermint oil “one of the most evidence-based herbal remedies in gastroenterology.” Dr. Lin Chang at UCLA points to 12 solid trials as proof. But not everyone’s convinced. Dr. Anthony Lembo from Harvard warns that recent high-quality trials show placebo effects may be stronger than we thought. The truth? Peppermint oil works for a lot of people-not everyone. But when it works, it works well. And because it’s not a drug, it’s worth trying if other options haven’t helped.
What to Look for When Buying
Not all peppermint oil is created equal. Here’s what to check:- Enteric coating: Non-coated capsules cause heartburn in 43% of users.
- Menthol content: Should be 50-65% (per European Pharmacopoeia).
- USP Verified: Only 62% of products on the market pass independent testing.
- Brand transparency: Avoid products that don’t list mg per capsule or menthol percentage.