Glaucoma damages the optic nerve and can steal vision slowly. Early stages often have no pain or obvious symptoms, so many people miss it. Regular eye checks with intraocular pressure and optic nerve exams catch it early. Treatment focuses on lowering eye pressure to slow damage.
Who’s at risk? People over 60, those with a family history, high eye pressure, certain ethnic groups (African or Latino ancestry), longstanding diabetes, and people who use steroid eye drops long-term. But anyone can get glaucoma.
Most people don't notice early vision loss because glaucoma first affects peripheral vision. When central vision is affected, damage is already advanced. Tests include tonometry (pressure), pachymetry (cornea thickness), visual field testing, optical coherence tomography (OCT) to measure nerve fiber layer, and a dilated eye exam.
Eye drops are the usual first step. Common classes are prostaglandin analogs, beta blockers, alpha agonists, carbonic anhydrase inhibitors, and Rho kinase inhibitors. Drops lower pressure by reducing fluid production or improving drainage. Take drops exactly as prescribed; missing doses can let pressure rise.
If eye drops don't work or side effects are bad, laser or surgery help. Laser trabeculoplasty improves drainage. Minimally invasive glaucoma surgeries (MIGS) lower pressure with less recovery time than traditional filtering surgeries. More advanced cases may need trabeculectomy or tube shunt surgery.
Medication-specific notes: prostaglandin drops (latanoprost, bimatoprost) usually cause fewer systemic side effects but can darken eyelashes and change iris color. Beta blockers (timolol) can affect heart and lungs — tell your doctor if you have asthma or heart disease. Oral carbonic anhydrase inhibitors may cause tingling, stomach upset, or kidney stones.
Lifestyle habits matter. Control blood sugar if you have diabetes, manage blood pressure, exercise moderately, eat a balanced diet with leafy greens and omega-3s, and avoid smoking. Protect your eyes from injury and wear safety goggles when needed.
Regular follow-up is crucial. Your eye doctor will track pressure, visual fields, and nerve imaging. If pressure creeps up or fields worsen, treatment changes quickly. Ask about side effects and cost; stick to the plan that fits your life.
When to see a doctor right away: sudden eye pain, sudden vision loss, halos around lights, nausea with eye pain, or a very red eye. Those could signal acute angle-closure glaucoma — an emergency.
Questions to ask your doctor: What is my target eye pressure? How often do I need tests? What are the side effects of my drops? Are there surgery options that fit my lifestyle? Knowing answers helps you stay in control.
Free resources: many national eye foundations offer clear guides, videos, and support groups. Ask your pharmacist about generic options — generics often cost less and work the same. If cost or access is a problem, check community clinics or patient assistance programs. Keep a medication list and bring your eye drop bottle to appointments. Small habits matter: set phone alarms for drops, keep a written schedule, and bring a family member to major visits so someone else knows the plan. You can protect your vision.
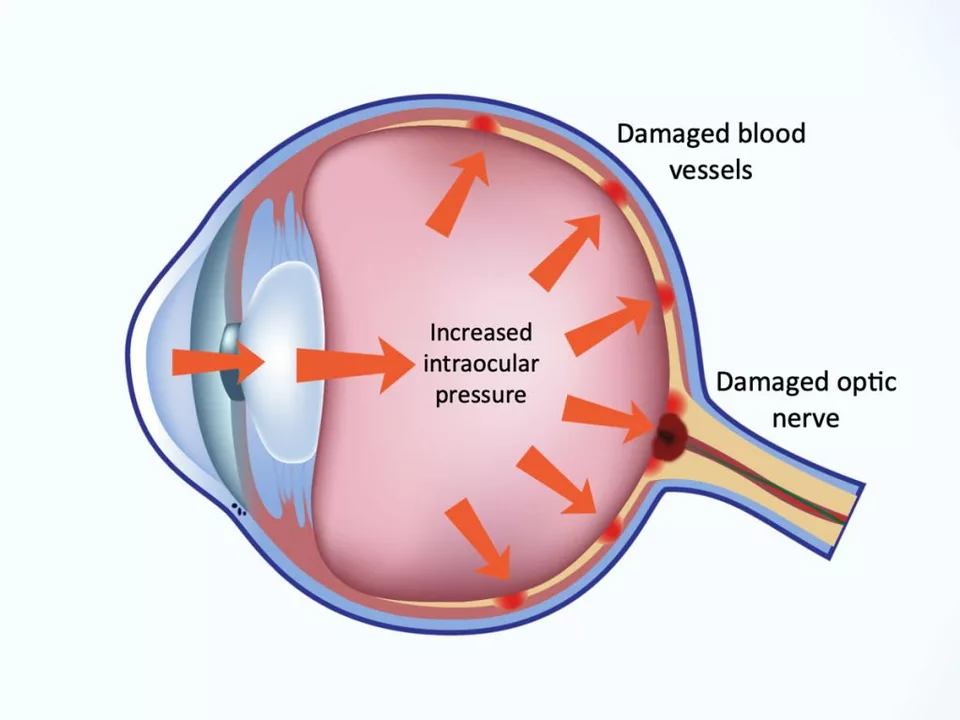
In a recent blog post, I discussed the link between high eye pressure and glaucoma, a potentially blinding eye disease. I learned that high eye pressure, also known as ocular hypertension, can damage the optic nerve and lead to glaucoma. It's important to have regular eye exams to detect any changes in eye pressure early on. While not everyone with high eye pressure will develop glaucoma, it is still a significant risk factor. Therefore, it's essential to be proactive in managing eye pressure and maintaining overall eye health.
Practical guide to using exercise to protect your liver with chronic hepatitis B-safe intensity, weekly plans, red flags, and what the science actually says.
Discover how evo-pharmacy.com is changing how Canadians get medications online: safe service, verified prescriptions, discreet delivery, and big savings compared to traditional drugstores.
Severe drug reactions can be deadly. Know the warning signs-like trouble breathing, skin peeling, or swelling-and act fast. Epinephrine saves lives in anaphylaxis. Delaying help can cost you yours.
Discover how butenafine works to clear jock itch quickly, why it outperforms other antifungals, and practical tips for safe use.
I recently discovered the incredible detoxifying effects of grapefruit dietary supplements and I'm amazed by the results! These supplements have not only helped me feel more energized, but also improved my digestion and overall health. I highly recommend giving grapefruit dietary supplements a try if you're looking to cleanse your body and boost your well-being. It's definitely a game changer in my daily routine. Don't miss out on experiencing these amazing benefits for yourself!