Understanding High Eye Pressure and Glaucoma
As someone who is always on the lookout for the latest information on eye health, I recently came across an important topic that I believe everyone should be aware of: the link between high eye pressure and glaucoma. In this article, I will discuss what high eye pressure is, how it is related to glaucoma, and what you can do to protect your eyes from this serious condition.
What is High Eye Pressure?
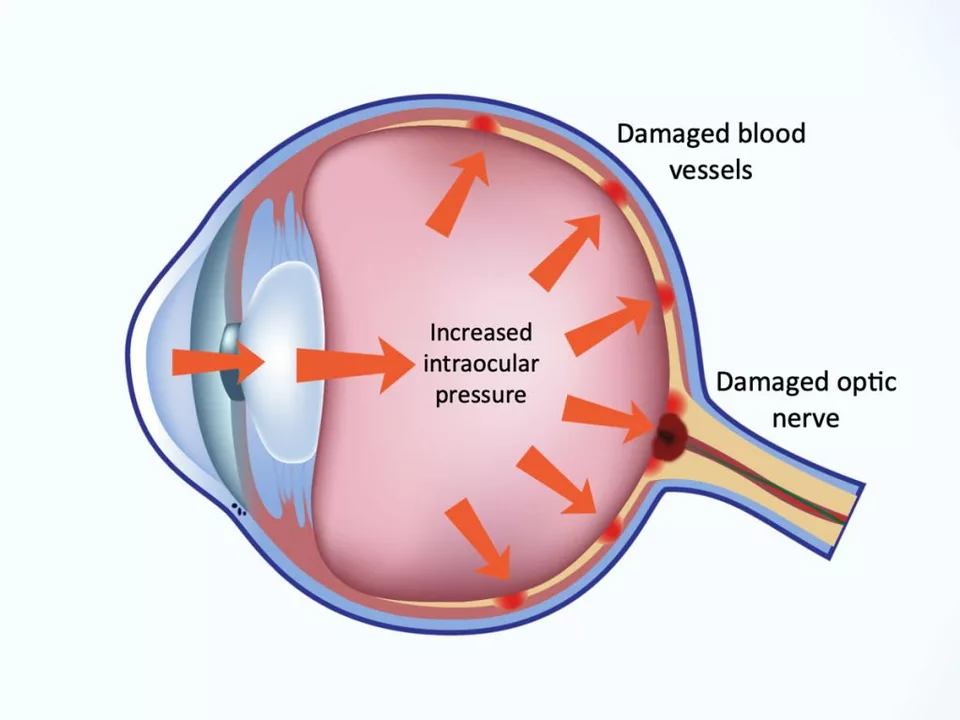
High eye pressure, also known as ocular hypertension, occurs when the fluid pressure inside your eyes increases. This fluid, called the aqueous humor, is essential for maintaining the health of your eyes, but when its pressure becomes too high, it can cause damage to the optic nerve and other parts of the eye. High eye pressure is not painful, and many people may not even be aware that they have it. However, it is important to get regular eye checkups to ensure the pressure remains within a healthy range.
What is Glaucoma?
Glaucoma is a group of eye diseases that can lead to irreversible vision loss and blindness. It is often associated with high eye pressure, although not everyone with high eye pressure will develop glaucoma. The most common form of glaucoma, called primary open-angle glaucoma, occurs when the eye's drainage system becomes blocked, leading to increased eye pressure and damage to the optic nerve. This damage can cause blind spots in your vision and, if left untreated, can result in complete vision loss.
How High Eye Pressure Increases the Risk of Glaucoma
Research has shown that high eye pressure is a major risk factor for developing glaucoma. As the pressure inside your eye increases, it can cause damage to the optic nerve, which is responsible for transmitting visual information from your eye to your brain. If the optic nerve becomes damaged, it can no longer effectively transmit this information, leading to a gradual loss of vision. While not everyone with high eye pressure will develop glaucoma, it is crucial to monitor and manage eye pressure to reduce the risk of this serious eye condition.
Diagnosing and Monitoring High Eye Pressure and Glaucoma
The only way to know if you have high eye pressure or glaucoma is through a comprehensive eye exam. During this exam, your eye doctor will measure your eye pressure using a device called a tonometer. They will also examine your optic nerve and perform additional tests to assess your vision and overall eye health. If your eye pressure is found to be higher than normal, your doctor may recommend additional testing and monitoring to determine if you are at risk for glaucoma. Regular eye exams are essential for early detection and treatment of both high eye pressure and glaucoma.
Treatment Options for High Eye Pressure and Glaucoma
If you are diagnosed with high eye pressure or glaucoma, your eye doctor will recommend a treatment plan to help manage your condition and prevent further vision loss. For high eye pressure, this may include prescription eye drops or oral medications to help lower the pressure inside your eyes. If you have glaucoma, your treatment plan may include medications, laser therapy, or surgery to improve the drainage of fluid from your eyes and reduce pressure. It is important to follow your doctor's recommendations and maintain regular eye exams to monitor your eye health and ensure the effectiveness of your treatment plan.
Protecting Your Vision: What You Can Do
As someone who cares about eye health, I cannot stress enough how important it is to take proactive steps to protect your vision. Regular eye exams are essential for detecting high eye pressure and glaucoma early on, giving you the best chance of preserving your vision. In addition to regular checkups, maintaining a healthy lifestyle – including a balanced diet, regular exercise, and avoiding smoking – can help reduce your risk of developing eye conditions like glaucoma. By taking care of your eyes and staying informed about eye health, you can help ensure a lifetime of clear, healthy vision.