Statins & ALS Risk Calculator
How Long Have You Taken Statins?
Your Personal Profile
Results will appear here after calculation
When you’re taking statins to lower your cholesterol, the last thing you want to hear is that they might be linked to ALS - a devastating, incurable neurodegenerative disease. The fear isn’t baseless. Since 2007, reports have surfaced linking statins to ALS, and some patients have stopped taking them out of concern. But here’s the truth: statins are not proven to cause ALS. In fact, the most rigorous studies suggest the opposite - long-term use might even protect against it.
Where Did the Fear Come From?
The alarm started with a spike in spontaneous reports to the U.S. Food and Drug Administration (FDA). People taking statins developed muscle weakness, fatigue, or trouble walking - symptoms that overlap with early ALS. When those symptoms appeared, some patients or doctors assumed the statin caused ALS. But correlation isn’t causation. In many cases, the muscle weakness was the first sign of ALS itself, not a side effect of the drug. Patients were already in the early, undiagnosed stages of the disease when they started statins - a phenomenon called reverse causality. In 2008, the FDA reviewed 41 large clinical trials involving thousands of patients. The results? No increase in ALS cases among statin users compared to those on placebo. The agency made it clear: don’t stop your statins because of ALS fears.What Do the Biggest Studies Say Today?
Fast forward to 2024, and the science has only gotten stronger. A major Norwegian study published in the European Journal of Neurology tracked 524 ALS patients over decades using national health registries. They found no link between statin use and ALS survival. The hazard ratio? 0.97 - meaning statin users lived just as long as non-users. The difference in survival time? Less than a month, and not statistically meaningful. The researchers concluded: “Statin use should not routinely be discontinued upon diagnosis.” Another 2024 study in Neurology dug deeper into timing. It found that people who started statins within a year before their ALS diagnosis had a higher risk - but only because they were already developing symptoms. The real surprise? Those who took statins for more than three years had a lower risk of developing ALS, especially men. This suggests long-term use might have a protective effect. Meanwhile, a controversial 2024 Mendelian Randomization study claimed massive risk increases for atorvastatin and rosuvastatin - with odds ratios so high (over 690,000 for rosuvastatin) that most experts dismissed them as statistically implausible. The method, which uses genetic data to infer causation, has known flaws when applied to drugs like statins. It’s not reliable enough to change clinical practice.Could Statins Actually Help?
The most surprising twist? Some lab studies suggest statins might slow ALS progression. In mouse models of ALS, lovastatin reduced disease risk by 28%. Atorvastatin cut motor neuron loss by 30%. How? By reducing inflammation in the brain and spinal cord. Statins lower not just cholesterol, but also inflammatory markers like CRP and IL-6 - both elevated in ALS patients. One 2018 study showed simvastatin suppressed harmful immune cells in the nervous system, potentially protecting neurons. Dr. Marc Weisskopf from Harvard, who led a 2022 study on long-term statin use, put it plainly: “Long-term use of statins had a protective role against the development and progression of ALS.”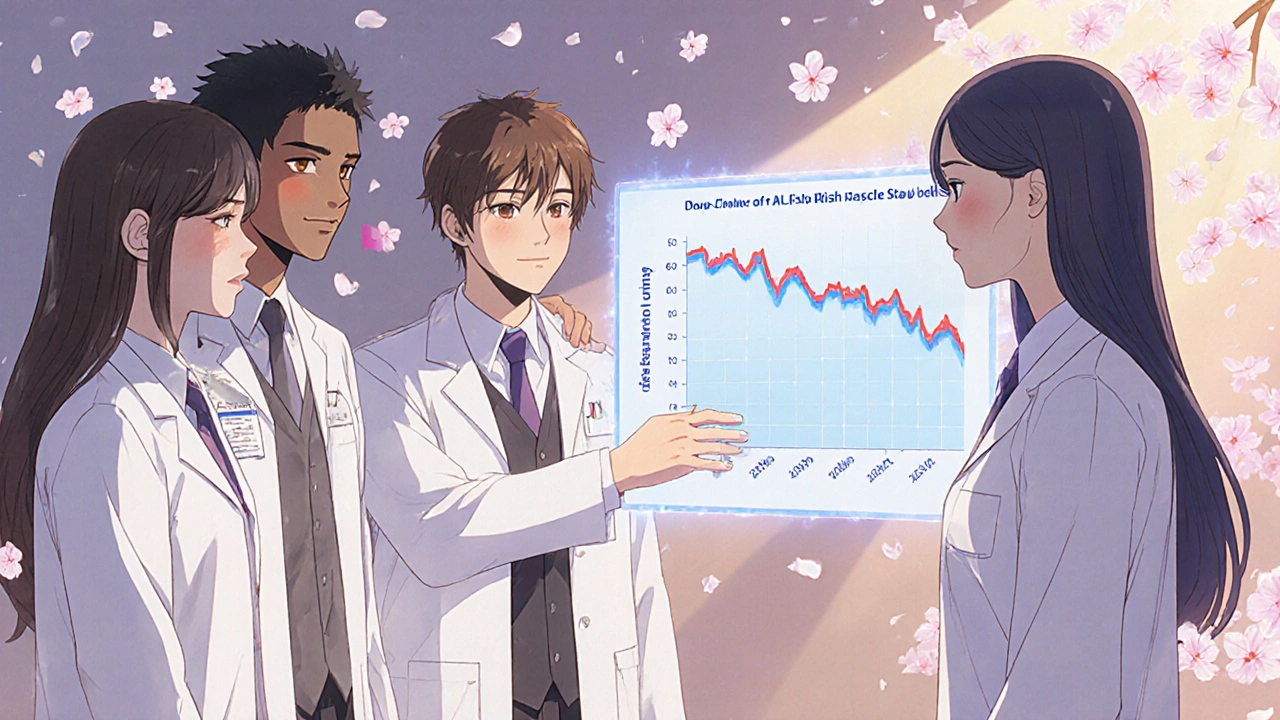
What Do Medical Experts Say Now?
Major health organizations are unified: - The Mayo Clinic (January 2024): “There’s no good evidence that statins cause or trigger ALS.” - The European Medicines Agency (June 2023): “Available evidence does not confirm a causal association.” - The American Heart Association: Still recommends statins as first-line therapy for high-risk patients. - The American Academy of Neurology (2023): “Statin therapy should be continued in ALS patients with established cardiovascular indications.” Even the FDA, which first raised the alarm in 2007, stands by its 2008 conclusion: “Healthcare professionals should not change their prescribing practices.”Why Do So Many Patients Stop Taking Statins?
The real danger isn’t the drug - it’s the fear. In the Norwegian study, 21% of ALS patients stopped statins in the year before diagnosis. Why? Because early ALS symptoms - muscle cramps, weakness, fatigue - feel exactly like common statin side effects. Doctors and patients misinterpret the signs. After diagnosis, another 12% stop statins based on rumors or online fears. But stopping can be dangerous. Many ALS patients have high cholesterol or heart disease. Stopping statins increases their risk of heart attack or stroke - problems that are preventable and often more immediate than ALS progression. Dr. Merit Cudkowicz of Massachusetts General Hospital says: “Many patients stop statins unnecessarily after an ALS diagnosis, which may put them at risk for preventable cardiovascular events.”
What Should You Do If You’re on Statins?
If you’re taking statins and have no ALS symptoms: keep taking them. The benefits for your heart far outweigh unproven neurological risks. If you’ve been diagnosed with ALS and are on statins:- Don’t stop unless your neurologist advises it.
- Discuss your cardiovascular risk - statins may still be critical for your long-term health.
- If you’re experiencing muscle pain, don’t assume it’s the statin. It could be ALS progression. Your doctor can test for it.
What’s Next in Research?
The CDC’s National ALS Registry is funding five new studies in 2025, including a 5-year trial tracking 10,000 statin users to see if long-term use truly lowers ALS risk. Results won’t be ready until 2030, but early data is already pointing toward benefit, not harm. Industry analysts predict that even if future studies show a tiny risk, statin use would drop by less than 5% - because the heart protection they offer is too valuable to give up.Bottom Line
Statins do not cause ALS. The evidence shows that. In fact, the longer you take them, the less likely you are to develop ALS - especially if you’re male. Early muscle symptoms don’t mean the drug is harming you; they might mean your body is already changing in ways that lead to ALS. If you’re worried, talk to your doctor. Don’t rely on social media posts or anecdotal stories. The science is clear: for the vast majority of people, statins are safe, effective, and possibly even protective.Don’t stop your statins because of fear. Stop them only if your doctor says it’s medically necessary.