DOAC Dosing Calculator for Renal Impairment
Calculate Kidney Function and DOAC Dosing
Cockcroft-Gault Creatinine Clearance:
0 mL/min
Apixaban Dosing Recommendation
Standard dose: 5 mg twice daily
DOAC Dosing Guidelines
Rivaroxaban
Use only if CrCl ≥ 15 mL/min. Do not use if CrCl < 15 mL/min.
Dabigatran
Use 75 mg twice daily if CrCl 15-30 mL/min. Do not use if CrCl < 15 mL/min.
Edoxaban
Use 30 mg daily if CrCl 15-50 mL/min. Do not use if CrCl < 15 mL/min.
Important Safety Note
The Cockcroft-Gault formula is essential for accurate DOAC dosing in renal impairment. Never rely solely on eGFR for DOAC dosing.
For apixaban: If two of the following apply - age ≥80, weight ≤60 kg, creatinine ≥1.5 mg/dL - use reduced dose of 2.5 mg twice daily.
Why DOACs Need Special Care in Kidney Disease
Direct Oral Anticoagulants, or DOACs, are the go-to blood thinners for millions of people with atrial fibrillation. They’re easier to use than warfarin-no weekly blood tests, fewer food interactions, and more predictable effects. But there’s a catch: if your kidneys aren’t working well, these drugs can build up in your body and turn dangerous.
Almost half of all patients on DOACs for AF have some level of kidney impairment. That’s not rare. It’s common. And when doctors don’t adjust the dose properly, the risks spike: too much drug means uncontrolled bleeding. Too little means clots, strokes, or heart attacks.
It’s not about avoiding DOACs. It’s about using them right. The key is matching the dose to how well your kidneys are filtering blood. And that’s not as simple as checking a lab report.
The Cockcroft-Gault Formula Isn’t Optional
Most doctors use eGFR to judge kidney function. It’s printed right on your lab results. But for DOACs, eGFR is misleading. The FDA, the American Heart Association, and the European Society of Cardiology all say: use the Cockcroft-Gault formula. Not eGFR. Not estimated GFR. Creatinine clearance.
The Cockcroft-Gault formula looks at your age, weight, sex, and serum creatinine. It’s old-developed in 1976-but it’s the only one validated for DOAC dosing. Why? Because it accounts for muscle mass. Older people, especially women and those who are thin, often have low muscle mass. Their creatinine drops, making eGFR look better than it is. But their kidneys might still be struggling to clear the drug.
For example: a 78-year-old woman, 52 kg, with a creatinine of 1.4 mg/dL might have an eGFR of 45 mL/min. But her Cockcroft-Gault CrCl could be just 28 mL/min. If you use eGFR, you might give her a full dose of rivaroxaban. That’s a recipe for internal bleeding.
Apixaban: The Safest Choice for Poor Kidneys
Among the four main DOACs, apixaban stands out. It’s the only one with enough data to support use even in end-stage kidney disease. While rivaroxaban, dabigatran, and edoxaban are off-limits below CrCl 15 mL/min, apixaban can still be used-just at a lower dose.
The standard dose is 5 mg twice daily. But if you meet any two of these three criteria: age 80 or older, body weight 60 kg or less, or serum creatinine 133 μmol/L (1.5 mg/dL) or higher-you drop to 2.5 mg twice daily. That’s it. No need to wait for CrCl to drop below 30. If you’re 82, weigh 55 kg, and have a creatinine of 1.6, you start on the lower dose.
Studies show apixaban reduces major bleeding by nearly 30% compared to warfarin in patients on dialysis. In one real-world study of 127 dialysis patients, the major bleeding rate was 1.8% with apixaban versus 3.7% with warfarin. That’s not just statistically significant-it’s life-changing.
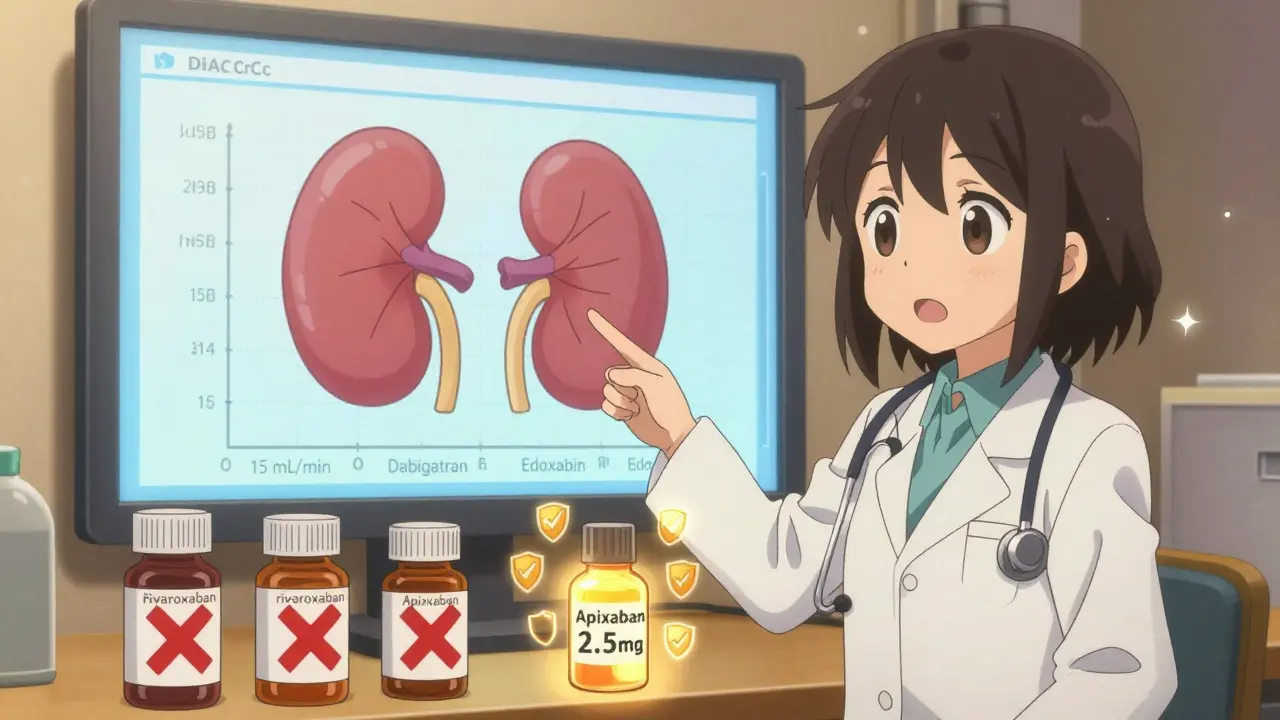
Rivaroxaban, Dabigatran, Edoxaban: Know the Limits
Don’t use rivaroxaban if your CrCl is below 15 mL/min. Period. Even 16 mL/min is too risky. It’s cleared mostly by the kidneys. When they fail, the drug stays in your system, thinning your blood too much.
Dabigatran needs a dose cut to 75 mg twice daily if CrCl is between 15 and 30 mL/min. Below that? No dose is safe. It’s not just about bleeding-it’s about losing control. One case report described a 76-year-old man on standard-dose dabigatran who bled into his brain after a minor fall. His CrCl was 12 mL/min. He wasn’t told to reduce the dose.
Edoxaban is easier: 60 mg daily becomes 30 mg daily if CrCl is between 15 and 50 mL/min. Below 15? Don’t use it. It’s not just guidelines-it’s evidence. The ENGAGE AF-TIMI 48 trial showed edoxaban’s effectiveness dropped sharply in patients with CrCl under 50. That’s not a gray area.
What Happens When Dosing Goes Wrong
A 2022 study in JAMA Internal Medicine found that 37.2% of DOAC prescriptions in patients with kidney disease were dosed incorrectly. That’s more than one in three. Why? Because it’s complicated.
Pharmacists see it every day. An elderly patient on apixaban 5 mg twice daily. They’re 81, weigh 58 kg, creatinine is 1.4. They’re on the wrong dose. No one checked the Cockcroft-Gault. No one noticed the weight. The doctor assumed eGFR was enough.
The consequences aren’t theoretical. GI bleeds. Intracranial hemorrhages. Emergency room visits. Deaths. One nurse in Ottawa told me about a patient who came in with black, tarry stools. His DOAC dose hadn’t been adjusted for his declining kidney function. He died within 48 hours.
It’s not about blame. It’s about systems. If your clinic doesn’t have a checklist, a pharmacist review, or a built-in alert in the EHR, you’re playing Russian roulette with someone’s life.

How to Get It Right Every Time
Here’s how to avoid mistakes:
- Always calculate CrCl using Cockcroft-Gault. Don’t rely on eGFR.
- For apixaban: if two of these apply-age ≥80, weight ≤60 kg, creatinine ≥1.5 mg/dL-use 2.5 mg twice daily.
- Never prescribe rivaroxaban if CrCl <15 mL/min. Avoid dabigatran and edoxaban below the same threshold.
- Recheck CrCl every 3 months in patients with CKD. Kidney function can change fast.
- Use the ABCs mnemonic: Age, Body weight, Creatinine. If two apply, reduce apixaban.
Many hospitals now use virtual anticoagulation clinics. These are teams-doctors, pharmacists, nurses-who review all anticoagulant prescriptions weekly. One study showed a 22.7% drop in bleeding events after they were implemented. That’s not magic. It’s teamwork.
The Future: What’s Coming by 2026
Right now, we’re flying blind in dialysis patients. The AXIOS trial was stopped early because too few people signed up. But the early data? Apixaban looked better than warfarin. The RENAL-AF trial is still running. Results expected in 2025 could finally give us clear answers for CrCl under 30 mL/min.
By 2026, we may have specific dosing rules for every stage of kidney disease. Until then, stick to the evidence. Apixaban at the reduced dose is your safest bet. Warfarin still has a role-but only when DOACs can’t be used safely.
Don’t assume. Don’t guess. Don’t use eGFR. Calculate CrCl. Check the criteria. Adjust the dose. It’s not complicated. It’s just not taught enough.
What About Patients on Dialysis?
Yes, DOACs can be used in dialysis patients-but only apixaban, and only at the reduced dose. Rivaroxaban, dabigatran, and edoxaban are not recommended. The data is limited, but what exists shows apixaban has the lowest bleeding risk.
Some nephrologists still use warfarin in dialysis because it’s been around longer. But studies show warfarin increases vascular calcification and intracranial bleeding in this group. Apixaban doesn’t. That’s why major guidelines now list apixaban as an option-even if the evidence isn’t perfect.
Bottom line: if you’re on dialysis and need a blood thinner, apixaban 2.5 mg twice daily is your best choice. But only if you’re also meeting the weight or age criteria. If not, you might still need the full dose. Talk to your doctor. Get the CrCl calculated. Don’t assume.