Storing medications safely in a shared living space isn’t just about keeping pills out of reach-it’s about preventing accidents, ensuring effectiveness, and avoiding legal trouble. Whether you’re living with aging parents, adult children, roommates, or in an assisted living facility, the way you store medicine can mean the difference between safety and disaster.
Why Medication Storage Matters More Than You Think
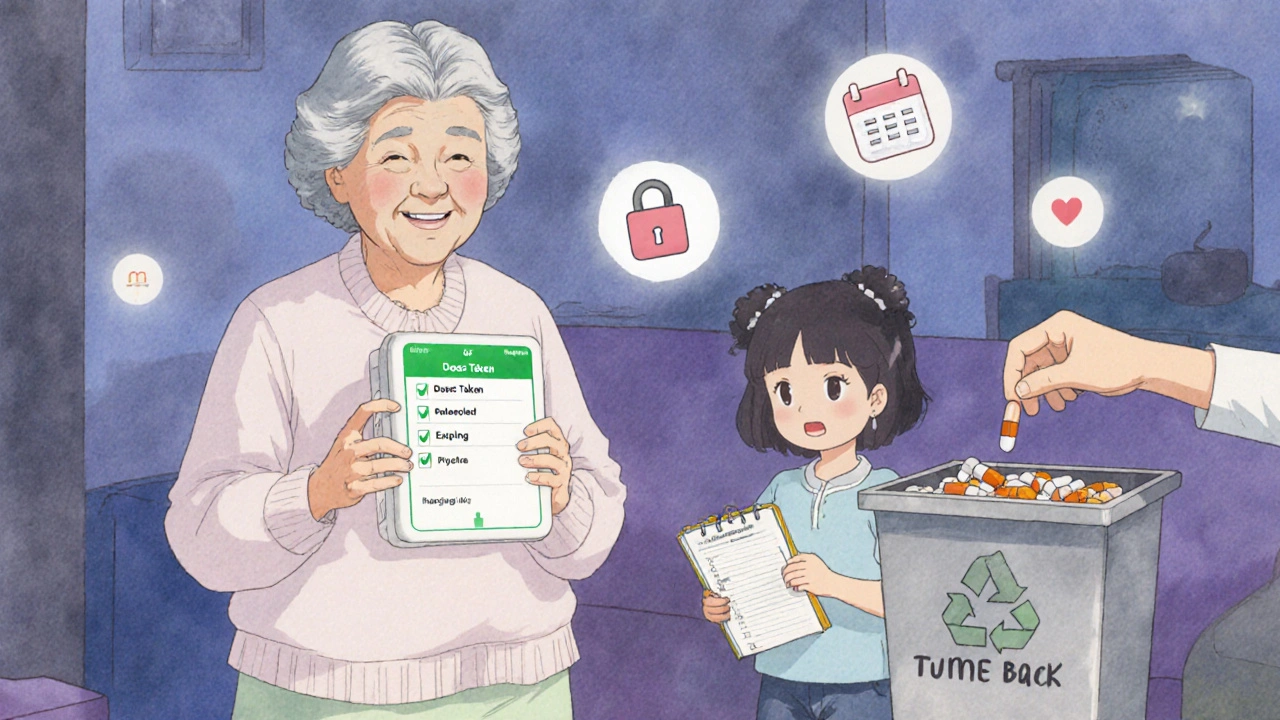
Every year, over 60,000 emergency room visits in the U.S. are caused by accidental medication ingestion by children under six, according to the CDC. In shared homes, that risk multiplies. A 2025 survey by SeniorHelpers found that 67% of multi-generational households had at least one medication-related incident in the past year. Most of these weren’t from intentional misuse-they were from someone grabbing the wrong bottle, leaving pills on a counter, or storing insulin on a fridge door where temperatures swing wildly. The Joint Commission found that between 2020 and 2021, 13% of hospitals received citations for improper medication storage. That’s not just a hospital problem. The same rules apply in homes where multiple people take medications. Temperature, access, labeling, and expiration dates all matter. A 2024 study from Johns Hopkins showed that certain antibiotics lose up to 30% of their potency after just 24 hours if stored above 77°F. That’s not theoretical-it’s what happens when you keep your blood pressure pills next to the toaster.Lock It Down: The First Rule of Safe Storage
If you’re sharing space with anyone who isn’t taking the same medications as you, every pill should be locked away. This isn’t optional. In regulated settings like assisted living facilities, 100% of homes are required to store medications in locked cabinets or carts. In homes, only 28% of families do it. You don’t need a fancy safe. A simple lockable medicine cabinet, a locked drawer in a bedroom dresser, or even a small lockbox bolted to the wall works. Keep it away from bathrooms-humidity ruins pills. Avoid kitchen counters. Don’t leave them on nightstands. Controlled substances like opioids, benzodiazepines, or stimulants require extra care. These are often targeted for misuse. In professional settings, access is logged. In homes, at least make sure only one person holds the key or combination. If you’re caring for someone with a history of substance use, consider a smart lockbox that records who opens it and when.Temperature Isn’t Just a Suggestion-It’s a Requirement
Not all meds need refrigeration, but the ones that do? They’ll fail if you store them wrong. Insulin, certain antibiotics, eye drops, and biologics must be kept between 36°F and 46°F. That’s fridge territory. But here’s the catch: the door of your fridge isn’t cold enough. The center shelves are. A 2024 case study from Eper.com showed a man’s insulin stopped working after three weeks on the fridge door-temperatures there fluctuated by 10°F daily. His blood sugar went wild. He didn’t know why until he checked the storage spot. If you’re sharing a fridge, use a small, labeled container and put it in the middle shelf, away from the freezer and the door. Label it clearly: “INSULIN - DO NOT TOUCH.” If you’re in a shared apartment and someone keeps moving your meds, get a mini-fridge just for medications. They’re cheap, quiet, and worth every dollar. The FDA updated its guidance in February 2024 for 47 commonly prescribed drugs, clarifying which ones need cold storage. Check the label or ask your pharmacist. If it says “store in refrigerator,” treat it like milk-not a suggestion.Label Everything-Even the Obvious
A 2021 Joint Commission survey found that 12% of hospitals got cited for poor medication labeling. That’s because people assume “the blue pill” means “blood pressure.” It doesn’t. One person’s blood pressure pill is another person’s anxiety med. Mix them up, and you’re risking a stroke, a fall, or worse. Use permanent markers and clear labels. Write the full name of the medication, the person’s name, and the dosage. If you’re using a pill organizer, label each compartment with the day and time. Don’t rely on color or shape. Pills change over time. Labels don’t. In assisted living facilities, medications often come in prepackaged bubble packs with names and times printed right on them. That’s the gold standard. If you’re managing meds at home, you can buy these packs from pharmacies for a small fee. Many offer weekly or monthly blister packs with your name, dosage, and schedule printed on each pill.
Clear Out the Clutter: Expired and Unused Meds Are a Hazard
Old meds are dangerous. They lose potency. They can be mistaken for new ones. And if they’re opioids or stimulants, they’re targets for theft. Every six months, do a full medicine cabinet audit. Toss anything that’s expired. That includes eye drops, cough syrup, and even vitamins. Most pills are good for 1-2 years past their expiration date, but that’s not a guarantee. Liquid meds? Throw them out on the date listed. They degrade fast. Don’t flush them. Don’t throw them in the trash unmarked. Use a drug take-back program. Many pharmacies, hospitals, and police stations in Canada and the U.S. offer free drop-off bins. In Ottawa, you can drop off unused meds at any participating Shoppers Drug Mart. The government runs a safe disposal program-use it.Separate Storage for Different Living Situations
Assisted living facilities handle meds differently than family homes. They use locked medication carts, daily MARs (Medication Administration Records), and trained staff. They’re audited. They’re held to strict standards. In a family home, you don’t need all that-but you need structure. Here’s how to adapt:- Multi-generational home: Keep all meds in one locked drawer in the bedroom of the person who manages them. No shared bathroom cabinets. No kitchen counters. Use a pill organizer with alarms if needed.
- Roommates: If you’re both on prescriptions, get two separate lockboxes. Label them clearly. No sharing. No borrowing. Even if you think your migraine pill is the same as theirs-it’s not.
- Living with a senior: If they’re forgetful, use a smart pill dispenser that beeps and locks until the right time. Some even call a family member if a dose is missed.
Documentation: The Quiet Hero of Medication Safety
In care homes, every pill given is recorded. Who gave it? When? Was it taken? That’s called a MAR. In homes, nobody writes it down-until something goes wrong. Start a simple log. A notebook or a free app like Medisafe or MyTherapy works. Write down:- Medication name
- Dosage
- Time taken
- Who gave it (if someone else is helping)
- Any side effects
What to Avoid
Here are the most common mistakes-and how to fix them:- Storing meds in the bathroom: Humidity ruins tablets. Move them to a bedroom drawer.
- Using the same container for multiple people: Even if the pills look alike, they’re not the same. Use separate labeled boxes.
- Leaving pills on the table during meals: That’s how kids grab them. Keep them locked until it’s time to take them.
- Ignoring expiration dates: Expired insulin, antibiotics, or epinephrine can be life-threatening.
- Assuming “everyone knows” where the meds are: Write it down. Show everyone. Don’t assume.
Tools That Actually Help
You don’t need high-tech solutions-but some tools make life easier:- Smart lockboxes (like DosePacker’s new model): Track access, monitor temperature, send alerts. $80-$150.
- Weekly pill organizers with alarms: Great for forgetful seniors. $15-$40.
- Mini-fridge for meds: Only if you need to refrigerate. Quiet, energy-efficient models cost under $100.
- Pharmacy blister packs: Many pharmacies now offer pre-sorted packs for $5-$10 per month. Worth it if you take five or more pills a day.
Final Thought: Safety Isn’t Complicated-It’s Consistent
Managing medication storage in a shared space isn’t about perfection. It’s about consistency. Lock it. Label it. Track it. Keep it cool. Toss the old stuff. Do it every day. The data doesn’t lie: households that use locked storage have 89% fewer incidents than those that don’t. The people who survive medication errors aren’t the ones who got lucky-they’re the ones who built systems. Start small. Pick one thing: lock the drawer today. Label the insulin tomorrow. Do the audit next weekend. You don’t need to fix everything at once. Just start.Can I store my medication in the same cabinet as my vitamins?
No. Vitamins and supplements aren’t regulated like prescription drugs, and mixing them increases the risk of accidental overdose or confusion. Keep all prescription and over-the-counter medications in a separate, locked container. Even if they’re both pills, treat them as different categories.
What if someone in the house doesn’t want their meds locked up?
It’s a common resistance, especially among older adults who value independence. But safety comes first. Explain that locking doesn’t mean distrust-it means preventing accidents. Offer a compromise: keep the key with them, but store it in a locked drawer they can access anytime. Many people feel better once they realize it’s about protection, not control.
Is it okay to use a pill organizer for all my meds?
Yes-if it’s used correctly. Pill organizers are great for daily routines, but don’t use them for meds that need refrigeration (like insulin) or for controlled substances unless you’re also locking the organizer. Always check with your pharmacist first. Some pills can’t be crushed or stored long-term in plastic compartments.
How do I dispose of old or expired medications safely?
Never flush them or throw them in the trash. Use a drug take-back program. In Ottawa, Shoppers Drug Mart and many police stations have free drop-off bins. You can also check Health Canada’s website for local collection events. If no option is available, mix pills with coffee grounds or cat litter in a sealed bag before trashing-but only as a last resort.
Do I need a special fridge just for medications?
Not always, but if you’re storing insulin, certain antibiotics, or biologics, yes. Shared fridges have temperature swings, especially near the door. A small, dedicated mini-fridge (under $100) with a thermometer inside gives you peace of mind. It’s cheaper than a hospital visit.







