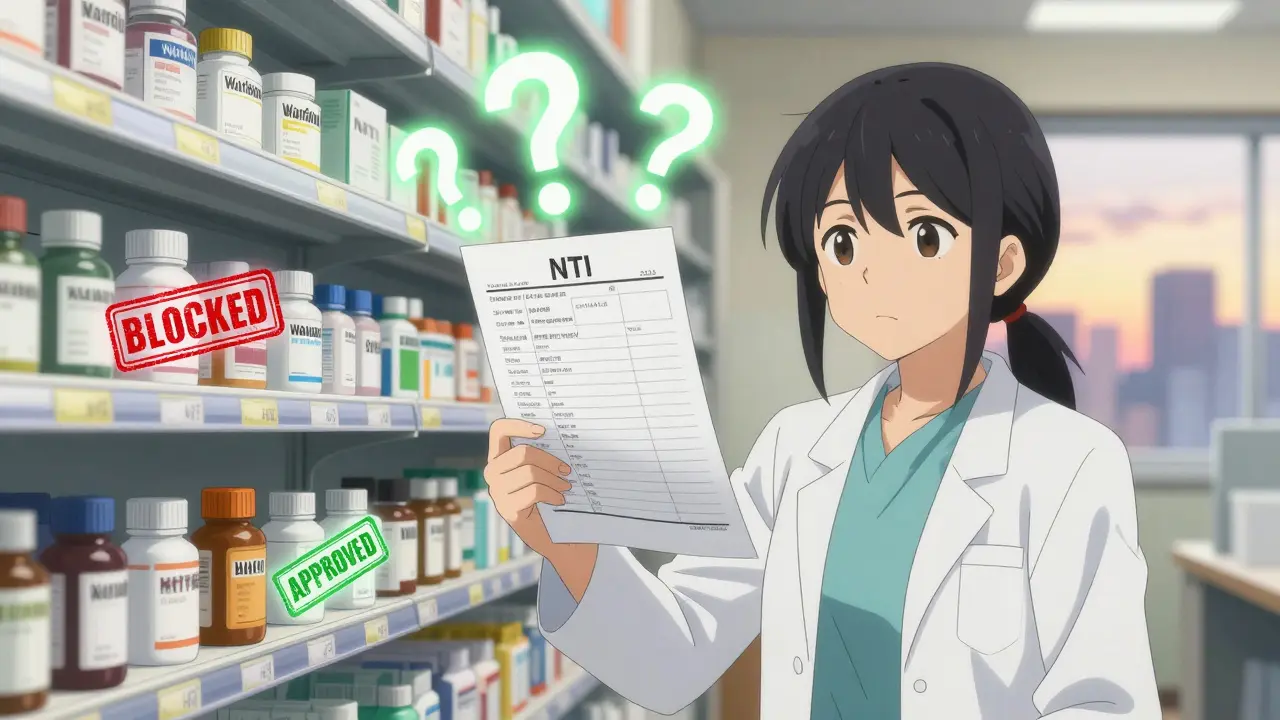
When you pick up a prescription for a medication like warfarin, levothyroxine, or lithium, you might assume that the generic version is just as safe and effective as the brand name. But in many states, that’s not automatically allowed. NTI drugs - those with a Narrow Therapeutic Index - are a special category where even tiny differences in dosage can lead to serious side effects or treatment failure. While the FDA says approved generics are just as safe, 27 states have their own rules that go further, restricting when and how pharmacists can switch a patient from brand to generic.
What Makes a Drug NTI?
NTI stands for Narrow Therapeutic Index. These are medications where the difference between a dose that works and a dose that’s dangerous is very small. Think of it like walking a tightrope - one step too far and you fall. Drugs like warfarin (a blood thinner), levothyroxine (for thyroid function), and lithium (for bipolar disorder) fall into this category. If the level in your blood is just a little too high, you could bleed internally. If it’s too low, you might get a clot, have a seizure, or experience a mood crash.
The FDA doesn’t officially label drugs as NTI. It doesn’t maintain a public list. But state pharmacy boards do. And they’ve built their own lists based on clinical reports, adverse event data, and expert opinion. That’s why one state might let you switch from brand to generic warfarin, while the next one requires your doctor to sign off every time.
How States Differ: Three Main Approaches
There’s no national standard. Instead, states have picked one of three main ways to handle NTI drug substitution:
- Carve-out provisions - These states simply say: “No substitution for these drugs.” Seventeen states take this route. Kentucky, for example, has a formal list of 27 NTI drugs that can’t be swapped without explicit written permission from the prescriber. That includes digoxin, levothyroxine, and lithium tablets. If a pharmacist tries to switch without approval, they’re breaking the law.
- Affirmative consent - Nine states require both the patient and the prescriber to give written permission before any substitution happens. North Carolina is one of them. The pharmacy must get signed consent from both parties before filling a refill for an NTI drug. This adds paperwork, time, and sometimes delays.
- Notification-only rules - Eleven states don’t block substitution, but they require the pharmacist to notify the prescriber (and sometimes the patient) within 72 hours after making the switch. Connecticut does this for anti-epileptic drugs. If the doctor or patient objects within 14 days, the substitution is canceled.
Some states mix these. For example, South Carolina doesn’t ban substitution outright but strongly recommends pharmacists avoid it for drugs like Synthroid and lithium. It’s advisory, not mandatory - but many pharmacists treat it like a rule anyway.
Which States Have the Strictest Rules?
Not all states are created equal. The most restrictive are:
- Kentucky - Maintains a detailed, legally binding list. Substitution is only allowed if the prescriber writes “substitution permitted” on the prescription. No exceptions.
- North Carolina - Requires dual consent: both patient and doctor must sign. The form must be kept on file for three years.
- Connecticut - For anti-epileptic drugs, substitution triggers a mandatory 72-hour notice. Either party can block it within 14 days.
On the other end of the spectrum, states like California, Texas, and Virginia follow the FDA’s lead. They treat NTI drugs like any other medication. If the generic is listed as therapeutically equivalent in the Orange Book, they allow substitution without extra steps.
Why the Confusion?
The tension comes from two different viewpoints.
The FDA says: “All approved generics meet the same standards. Bioequivalence testing proves they’re the same.” And they’re right - in controlled studies, generic warfarin and brand warfarin show nearly identical blood levels.
But clinicians see something else. A 2020 study in Circulation: Cardiovascular Quality and Outcomes found no significant difference in INR stability between brand and generic warfarin in over 12,000 Medicare patients. Yet pharmacists in Kentucky report that patients on levothyroxine who were switched to a different generic often come back with symptoms of under- or over-treatment - fatigue, heart palpitations, weight changes.
Dr. Aaron Kesselheim, a Harvard researcher who studied state NTI laws, says: “The data isn’t perfect, but when you’re dealing with drugs where a 10% difference in absorption could mean hospitalization, it’s not crazy to ask for extra caution.”
Meanwhile, the Association for Accessible Medicines argues that many drugs on state NTI lists don’t even have solid evidence of a narrow index. They point out that only 12 of the 47 drugs on state lists have been confirmed as truly NTI through systematic review.
Real-World Impact: Time, Cost, and Workflow
These rules aren’t just paperwork - they change how pharmacies operate.
In states with carve-outs or consent rules, pharmacists spend an average of 3.2 minutes per prescription just checking if substitution is allowed. In states without restrictions, it’s under a minute. That adds up. One pharmacist in Kentucky told a survey: “I lose 5 to 7 minutes on every NTI script. That’s 20 extra hours a month.”
Chain pharmacies use software that auto-checks state-specific NTI lists. Independent pharmacies? Many still use printed lists or manual lookup tools. That’s why substitution rates for NTI drugs are 37% lower in states with strict rules - not because patients refuse, but because the system slows it down.
Cost-wise, states with restrictive laws have 12.4% lower generic use for NTI drugs. That means more patients pay full price for brand-name versions. In 2022, NTI drugs accounted for $28.7 billion in U.S. prescriptions. Even a small drop in generic use adds up.
What’s Changing?
The landscape is shifting. California passed a law in 2022 requiring any NTI designation to be based on scientific evidence - not tradition. New York and Ohio are reviewing their lists using the FDA’s new 2023 draft guidance, which suggests a clearer threshold: a drug is NTI if the ratio between its toxic and effective dose is 2.0 or less.
The National Association of Boards of Pharmacy is working on a model framework to bring some consistency. But don’t expect uniformity soon. States see this as a public health issue - and they’re not giving up control.
And legal challenges are growing. In 2023, the Association for Accessible Medicines sued Kentucky, arguing its NTI list creates an “undue burden on interstate commerce.” The case is still pending. If it goes the right way, it could force states to justify their rules with hard data - not fear.
What Should You Do?
If you’re on an NTI drug:
- Ask your pharmacist: “Is this medication on my state’s restricted list?”
- Check your prescription label - some states require a note like “Do Not Substitute” if the drug is on the list.
- If you’re switched to a generic and feel different - fatigue, dizziness, irregular heartbeat - contact your doctor immediately. Even if your state allows substitution, your body might not respond the same way.
- Know your rights. In states with consent rules, you can refuse substitution - even if your doctor says yes.
If you’re a prescriber:
- Know your state’s rules. A prescription that says “Dispense as written” might be required for NTI drugs in your area.
- Use electronic prescribing - it can auto-flag NTI restrictions based on state law.
- Document your reasoning. If you approve substitution, write why. It protects you and the patient.
Which states prohibit generic substitution for NTI drugs entirely?
Kentucky, North Carolina, and Connecticut are among the strictest. Kentucky has a formal list of 27 drugs where substitution is banned unless the prescriber writes explicit permission. North Carolina requires written consent from both patient and prescriber. Connecticut prohibits substitution for anti-epileptic drugs unless both parties are notified and don’t object within 14 days.
Are all generic NTI drugs unsafe?
No. The FDA requires all approved generics to meet the same bioequivalence standards as brand-name drugs. Studies show most generic NTI drugs perform just as well. But because these drugs have very little room for error - even small differences in absorption can matter - some states and clinicians prefer extra caution. It’s not about safety of generics overall, but about minimizing risk in high-stakes situations.
Can I ask my pharmacist not to substitute my NTI drug?
Yes. Even in states without restrictions, you can request the brand name. In states with consent rules, you have the legal right to refuse substitution. Tell your pharmacist you want to stay on your current version. They’ll honor it. If they push back, ask to speak with the pharmacy manager - this is a patient right.
Why do some states list Synthroid and Premarin as NTI drugs?
Synthroid (levothyroxine) and Premarin (conjugated estrogens) are on many state lists because of anecdotal reports of patients experiencing symptoms after switching. While clinical studies show little difference in blood levels, some patients report fatigue, weight changes, or mood shifts. States respond to these reports - even if the evidence isn’t conclusive - because the consequences of failure (like thyroid storm or stroke) are severe.
Is there a national NTI list I can check?
No. The FDA does not maintain a public NTI list. The closest thing is the Orange Book, which lists therapeutic equivalents - but doesn’t flag NTI drugs. To find your state’s rules, check your state board of pharmacy website. Most have a section on generic substitution or NTI policies. Some even post downloadable lists.