Why Your Monthly Pharmacy Trips Are Costing You More Than You Think
If you’re juggling three or more prescriptions, you’ve probably noticed something frustrating: each refill feels like a separate bill. One month you pay $15 for blood pressure meds, then $20 for diabetes pills, then $30 for cholesterol medicine - all on different days. That’s not just inconvenient. It’s expensive. Every trip to the pharmacy means another copay, another out-of-pocket hit. And if you’re on Medicare or a tiered insurance plan, those copays add up fast.
Here’s the truth: you don’t have to pay that way. There’s a simple, free service most pharmacies offer that can cut your visits in half - and your copays by hundreds a year. It’s called medication synchronization, or med sync. And it’s not some fancy tech gadget or new drug. It’s just smarter scheduling.
What Is Medication Synchronization? (And Why It Works)
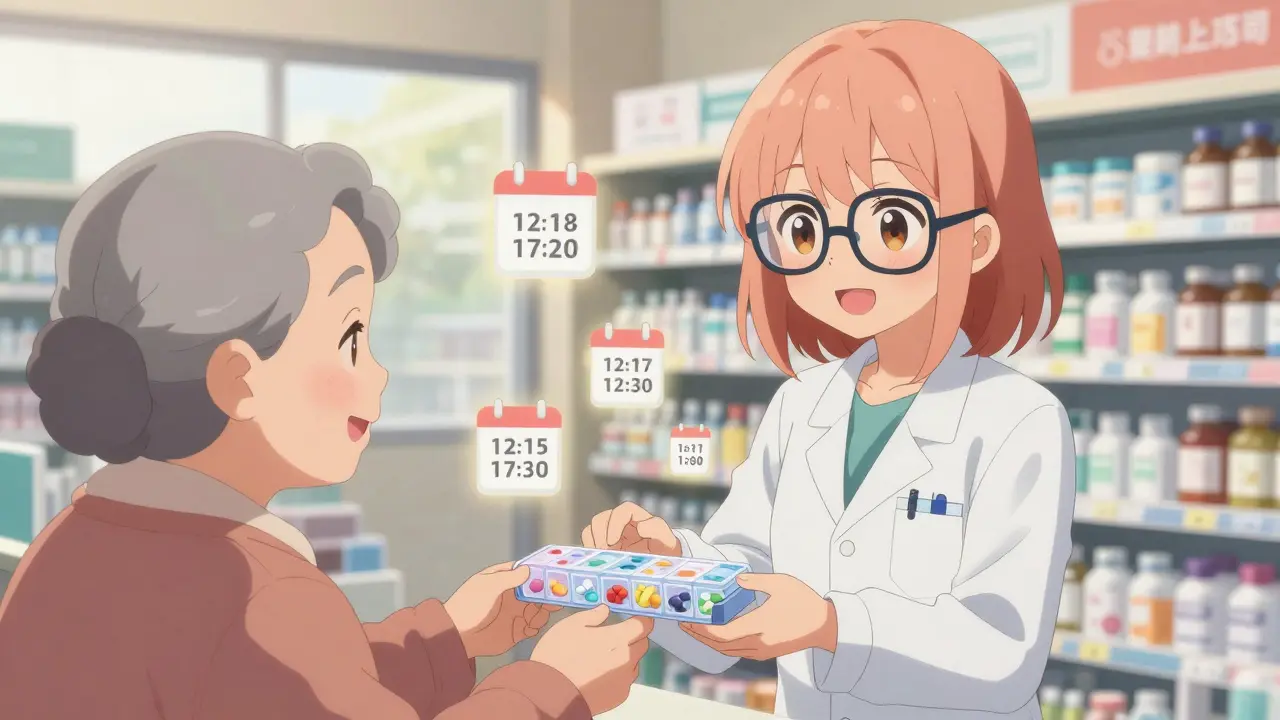
Med sync is when your pharmacy aligns all your chronic medications to refill on the same day each month. Instead of picking up your blood pressure pills on the 5th, your insulin on the 12th, and your arthritis med on the 20th, you walk in once - say, the first Tuesday of every month - and leave with everything you need.
This isn’t just about convenience. It’s about money. Every time you refill a prescription, you pay a copay. If you’re on a three-tier plan (common with Medicare Part D), those copays can be 57.6% higher per prescription than on simpler plans. And if you’re refilling six meds a month? That’s six copays. Switch to med sync, and you’re down to one. That’s not a small saving - it’s often $100 to $200 a year just from fewer transactions.
But here’s the real win: better adherence. A 2021 study by the Institute for Safe Medication Practices found medication errors increase by 32% when patients manage multiple, staggered refill dates. Missed doses, wrong timing, confusion over what to take when - all of it goes down when everything syncs up. CMS data shows patients using med sync have 23.6% fewer hospital visits due to medication problems.
How to Get Started: The Four-Step Process
Getting set up is easier than you think. You don’t need a doctor’s note or special approval. Just walk into your pharmacy and ask.
- Ask for med sync - Tell the pharmacist you want all your chronic meds synced to one day. They’ll check your list and see if it’s possible. Most major chains - CVS, Walgreens, Shoppers Drug Mart - offer this for free.
- Get a full med review - The pharmacist will look at everything you’re taking, including over-the-counter pills and supplements. This isn’t just for syncing - it’s a safety check. They might spot duplicates, interactions, or meds you don’t need anymore.
- Adjust your refills - This is the trickiest part. If one med is due in 10 days and another in 45, the pharmacy will give you a short-term supply (a “short fill”) to bring all dates together. You might get a few extra pills one month, or a slightly smaller dose the next. It’s temporary. Most programs take 1 to 3 months to fully sync.
- Pick up on your day - Once synced, you’ll get a reminder (text, call, or app notification) when your meds are ready. Show up once a month. Done.
Some people worry about running out of meds during the transition. That’s normal. But the pharmacy will make sure you’re covered. If you’re short for a few days, they’ll give you a small emergency supply. Talk to them - don’t guess.
What If Your Insurer Makes It Hard?
Med sync doesn’t change your copay amount - just how often you pay it. But there’s another hidden cost: copay accumulators.
Since 2017, many insurers have started using copay accumulator programs. Here’s how they work: if you use a manufacturer coupon (like a $500 card for a specialty drug), the insurer won’t count that toward your deductible. So even if you’ve spent $5,000 on copays using coupons, your deductible might still be $0. That means when your coupon runs out, you’re stuck paying full price.
One Reddit user in Ottawa shared: “My $5,000 manufacturer coupon for my MS drug got voided by my plan. My monthly cost jumped from $50 to $650. I had to choose between meds and groceries.”
If you’re on a specialty drug - things like biologics for rheumatoid arthritis, multiple sclerosis, or cancer - this is critical. Ask your pharmacist: “Does my plan use copay accumulators?” If yes, ask if they can help you find alternative funding. Some manufacturers now offer direct financial aid or patient assistance programs that bypass the accumulator issue entirely.

Combination Pills: The Ultimate Shortcut
Some meds come combined - one pill with two or more drugs inside. For example, a single tablet might contain a blood pressure medicine and a water pill. These are called fixed-dose combinations.
If your doctor can switch you to one of these, you cut your pill count - and your copays - in half. MaxCareRx found that patients on combination pills had up to 27% fewer missed doses. Between 2018 and 2023, the FDA approved 127 new combination medications. Ask your doctor: “Are there any combo pills that work for my condition?”
Not every med has a combo version. But for diabetes, high blood pressure, and cholesterol, there are plenty. And if one exists, it’s often cheaper than buying two separate pills.
When Med Sync Won’t Work (And What to Do Instead)
Med sync isn’t perfect. Some meds can’t be synced:
- Drugs that need to be taken daily (like antibiotics or short-term pain meds)
- 90-day supplies (if your plan only allows 30-day refills)
- Medications with strict refill rules (e.g., controlled substances)
For these, you still need to manage separate refills. But here’s a pro tip: ask your pharmacist if you can get a 90-day supply of your maintenance meds. Many plans let you do this for chronic conditions - and you’ll pay only one copay instead of three. That’s a big win.
If your plan blocks early refills, you’re not stuck. Pharmacists can request “early refill exceptions” for patients with sync needs. It’s not automatic, but it’s common. Just ask.
Real Results: What People Are Saving
A 72-year-old woman in Mississauga was taking eight meds, refilled on eight different days. She was paying $180 a month in copays - $2,160 a year. After syncing with her local pharmacy, she now pays $60 a month - $720 a year. She saved $1,440. And she stopped missing doses.
Another man in Hamilton was on a specialty drug with a $50 copay and a $500 manufacturer coupon. His insurer’s accumulator program made the coupon useless. He switched to a patient assistance program offered by the drugmaker. His cost dropped to $10 a month. He didn’t change his meds. He just changed how he paid.
These aren’t outliers. Walgreens’ med sync program has 1.2 million users. CVS has over 4 million. That’s not marketing fluff - that’s real people saving money and staying healthy.

What You Should Do Right Now
You don’t need to wait for a doctor’s appointment or a new insurance card. Start today:
- Write down every prescription you take - including doses and refill dates.
- Call or visit your pharmacy. Ask: “Can you sync my medications?”
- Ask: “Do you know if my plan uses copay accumulators?”
- Ask: “Are there any combination pills I could switch to?”
- Ask: “Can I get a 90-day supply of my maintenance meds?”
If your pharmacy says no, try another one. Not all pharmacists know how to do this well. But most will try. And if they don’t, ask to speak to the pharmacist in charge - they’re the ones who run the program.
What’s Changing in 2025
The government is starting to act. The 2025 Medicare Part D proposed rule will limit how insurers use copay accumulators. The HHS estimates this will save patients $1,200 a year on average. That’s huge.
Meanwhile, pharmacies are rolling out digital tools. Apps now send refill reminders, track your adherence, and even notify your doctor if you miss a dose. The FDA has cleared 63 such apps. Some are free. Ask your pharmacist which ones they recommend.
By 2030, experts predict 95% of chronic medication management will use some form of coordination. The goal isn’t just to save money - it’s to keep people out of the hospital.
Final Thought: Your Meds Are Your Health
It’s not about being lazy. It’s about being smart. Managing multiple prescriptions is hard. The system wasn’t built for it. But you don’t have to fight it alone. Your pharmacist isn’t just someone who hands out pills - they’re your ally in staying healthy and saving money.
One sync appointment. One conversation. One less trip to the pharmacy every month. That’s all it takes to cut your copays and your stress.