Pain-Lung Connection Symptom Checker
This tool helps you assess whether your symptoms might indicate a connection between chronic pain and lung inflammation. Based on the article content, check the symptoms you experience and get personalized information about potential links.
Select Your Symptoms
Key Takeaways
- Chronic pain and lung inflammation often share underlying immune pathways, especially inflammatory cytokines.
- Conditions like COPD, asthma, and fibromyalgia illustrate how persistent pain can arise from or worsen respiratory inflammation.
- Identifying overlapping symptoms (e.g., shortness of breath, chest tightness) helps clinicians catch the link early.
- Lifestyle changes, anti‑inflammatory diets, and targeted therapies can reduce both pain and lung irritation.
- Ongoing research points to nerve‑immune cross‑talk as a promising treatment target.
What Is Chronic Pain?
When discussing health, Chronic Pain is a persistent pain condition lasting longer than three months, often without a clear injury. It affects roughly 20% of adults worldwide, according to the World Health Organization's 2023 survey. Unlike acute pain, which warns us of tissue damage, chronic pain becomes a disease in its own right, rewiring the nervous system and keeping inflammatory pathways turned on.
What Is Lung Inflammation?
Similarly, Lung Inflammation is the swelling and irritation of lung tissue caused by immune cells, pollutants, infections, or autoimmune activity. It shows up as bronchitis, asthma attacks, or the chronic changes seen in COPD. In 2024, the Global Burden of Disease report listed lung inflammation‑related disorders as the third leading cause of disability-adjusted life years (DALYs) globally.
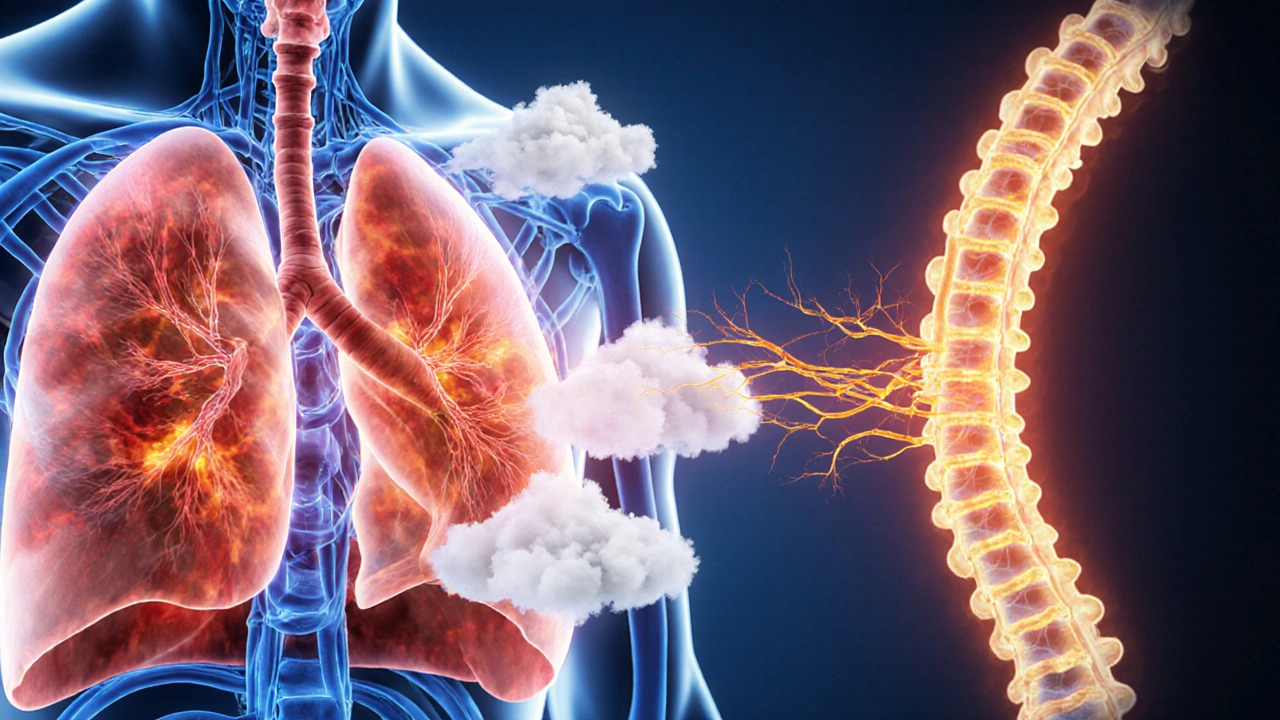
How the Two Conditions Intersect
At first glance, pain that sticks around for months and inflamed lungs seem unrelated. The bridge is the body's immune system. When the lungs inflame, they release inflammatory cytokines such as IL‑6, TNF‑α, and IL‑1β. These molecules travel through the bloodstream and can sensitize peripheral nerves, a process called nerve sensitization. Sensitized nerves fire more easily, turning mild discomfort into a chronic ache.
Conversely, sustained pain triggers the sympathetic nervous system, raising cortisol and other stress hormones. Over time, this hormonal surge can impair lung function, making the airways more reactive to irritants. In short, it’s a two‑way street where each condition fuels the other.

Key Biological Players
Understanding the overlap requires a look at the main actors:
- Inflammatory cytokines - messengers that amplify both pain and lung swelling.
- Oxidative stress - free radicals that damage nerve endings and lung tissue alike.
- Microglia - immune cells in the spinal cord that keep pain circuits on high alert.
- Pulmonary fibroblasts - cells that remodel lung architecture during chronic inflammation, contributing to stiffness and pain.
- TRP channels - protein doors on nerve cells that open in response to heat, chemicals, or acidity, linking respiratory irritants to pain signals.
Common Conditions Where the Link Shows Up
Several medical diagnoses illustrate the chronic‑pain‑lung‑inflammation connection:
| Condition | Primary Pain Feature | Respiratory Inflammation Aspect | Typical Overlap Mechanism |
|---|---|---|---|
| Chronic Obstructive Pulmonary Disease (COPD) | Chest tightness, rib‑cage muscle fatigue | Persistent bronchial inflammation | Cytokine spill‑over sensitizes intercostal nerves |
| Asthma | Exercise‑induced muscle aches | Eosinophilic airway inflammation | IL‑5 driven eosinophils release nerve‑activating mediators |
| Fibromyalgia | Widespread musculoskeletal pain | Often co‑exists with low‑grade lung inflammation | Systemic cytokines lower pain thresholds |
| Pulmonary Fibrosis | Sharp pleuritic pain | Scarring and stiffening of lung tissue | Fibroblast‑derived growth factors irritate visceral nerves |
| Chronic Bronchitis | Upper‑body ache from coughing | Excess mucus and airway wall thickening | Repeated cough stress triggers peripheral nerve hyper‑responsiveness |
Spotting the Overlap: Symptoms to Watch For
If you or a patient experiences any of the following, consider a shared pathway:
- Persistent chest discomfort that worsens after a coughing episode.
- Shortness of breath paired with generalized body aches or fatigue.
- Morning stiffness that improves with deep breathing exercises.
- Frequent headaches that coincide with wheezing or nocturnal coughing.
- Elevated resting heart rate alongside unexplained muscle soreness.
These patterns often hint at cytokine‑mediated nerve sensitization. A simple blood test for C‑reactive protein (CRP) or IL‑6 can flag systemic inflammation, prompting a deeper look at both pain and lung health.
Managing Both Sides of the Equation
Because the root cause sits in the immune system, treatments that target inflammation can relieve both pain and breathing trouble.
- Anti‑inflammatory medication: Low‑dose naltrexone, certain NSAIDs, and corticosteroid bursts (used sparingly) have shown dual benefits in small 2022 clinical trials.
- Physical therapy: Guided breathing exercises improve diaphragm mobility, reducing rib‑cage strain and cutting down pain signals.
- Dietary changes: A Mediterranean‑style diet rich in omega‑3 fatty acids cuts IL‑6 levels by up to 30% (meta‑analysis, 2023).
- Mind‑body techniques: Mindfulness‑based stress reduction lowers cortisol, which in turn calms both nerve excitability and airway hyper‑reactivity.
- Targeted biologics: For patients with high eosinophils, drugs like mepolizumab block IL‑5, easing asthma attacks and associated musculoskeletal pain.
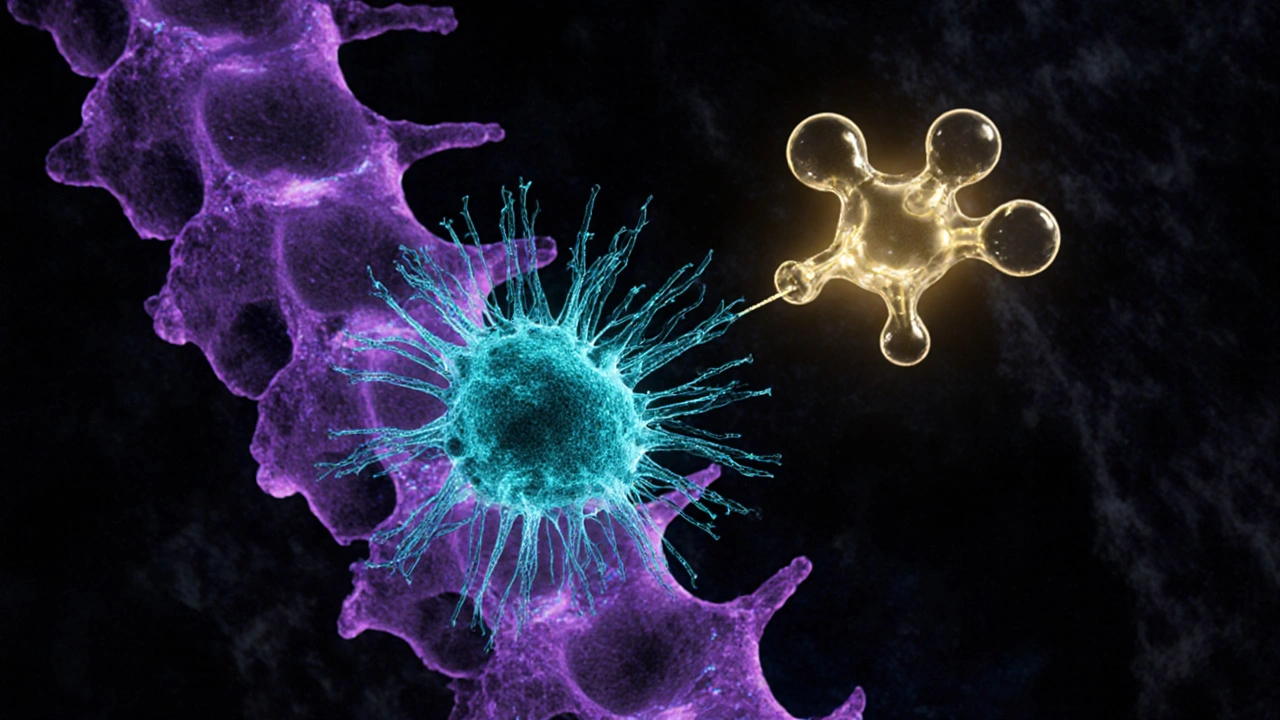
Emerging Research: The Nerve‑Immune Interface
Scientists are zeroing in on the concept of a "neuro‑immune synapse"-the point where immune cells and nerve endings directly talk. A 2024 study from the University of Toronto used advanced imaging to show microglia extending fingers toward spinal dorsal horn neurons after mice inhaled cigarette smoke. Blocking the P2X7 receptor stopped both lung inflammation and the development of chronic pain behaviors.
Another promising avenue is the use of TRP channel antagonists. Early‑phase trials report that oral capsazepine reduced cough‑related chest pain by 45% without major side effects.
Practical Checklist for Patients and Clinicians
- Ask about recent respiratory infections or exposure to pollutants when evaluating chronic pain.
- Include spirometry or peak flow measurements in pain assessments for at‑risk individuals.
- Order a basic inflammatory panel (CRP, ESR, IL‑6) if pain appears out of proportion to injury.
- Start a low‑impact aerobic program (e.g., walking, swimming) to improve lung capacity and release endorphins.
- Review medication lists for drugs that may exacerbate inflammation, such as certain opioids or high‑dose NSAIDs.
Frequently Asked Questions
Can chronic pain cause lung problems on its own?
Pain itself doesn’t damage lung tissue, but the stress response it triggers can increase airway reactivity. Over time, this may worsen pre‑existing conditions like asthma.
Is it safe to take anti‑inflammatory drugs if I have a chronic lung disease?
Short courses of NSAIDs are generally safe, but long‑term use can irritate the stomach and affect kidney function, which in turn may influence fluid balance in the lungs. Always discuss duration and dosage with a physician.
What lifestyle changes help both conditions?
Quit smoking, reduce exposure to indoor pollutants, maintain a balanced anti‑inflammatory diet, stay active with low‑impact cardio, and practice stress‑reduction techniques such as yoga or meditation.
Are there any specific supplements that aid both pain and lung health?
Omega‑3 fish oil, curcumin, and vitamin D have shown modest reductions in systemic inflammation and can improve respiratory function in deficient individuals.
How quickly can one expect improvement after starting treatment?
Results vary. Anti‑inflammatory meds may relieve symptoms within days, while lifestyle changes and biologics often take 4‑12 weeks to show measurable benefits.
Bottom Line
The next time you hear someone complain of chronic aches alongside a cough, remember that chronic pain and lung inflammation often travel together on the same inflammatory highway. By spotting the link early and treating the root immune drivers, patients can break the cycle, breathe easier, and live with less pain.