Unlocking the Potential of Cycloserine in MDR-TB Treatment
As multidrug-resistant tuberculosis (MDR-TB) continues to pose a significant global health challenge, it is crucial to explore new and effective treatment options. One such promising candidate is cycloserine, a second-line antibiotic that has shown potential in managing MDR-TB. In this section, we will delve into the history, properties, and potential uses of cycloserine in the fight against MDR-TB. We will also discuss the recent advancements in research and development surrounding this critical antibiotic.
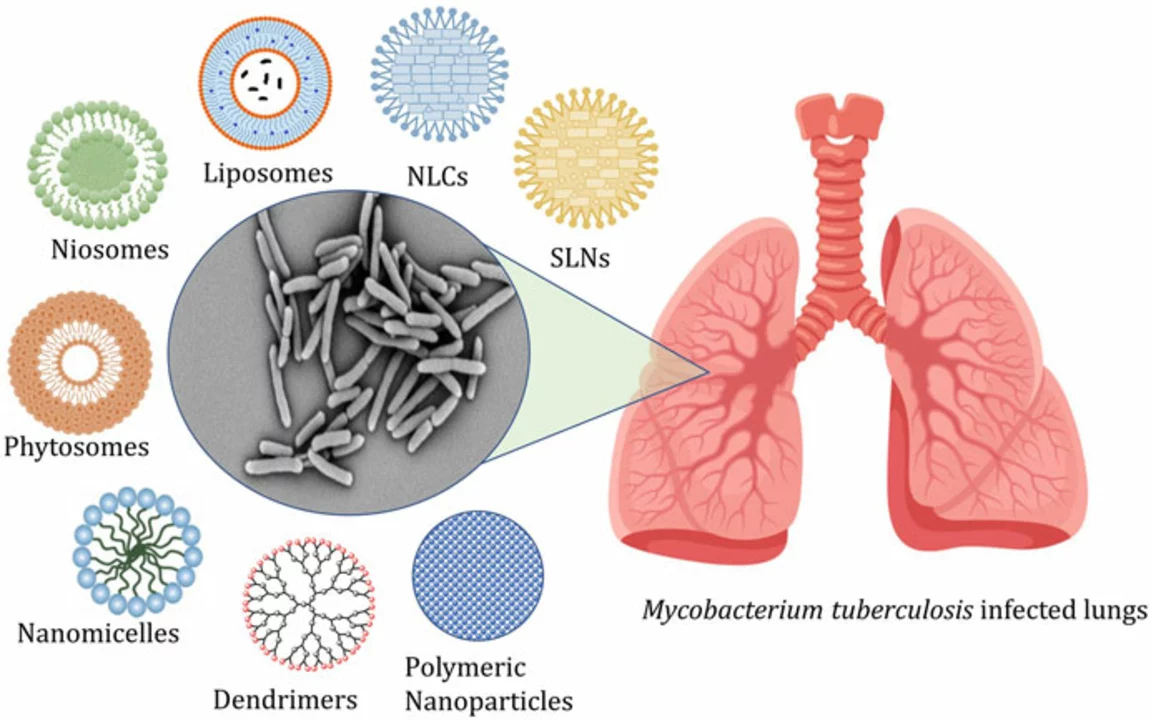
From its initial discovery in the 1950s as a byproduct of Streptomyces orchidaceus, cycloserine has come a long way in terms of its usage and efficacy. It works by inhibiting the synthesis of the bacterial cell wall, thereby making it difficult for the Mycobacterium tuberculosis to grow and reproduce. Recent research has shed light on the potential of cycloserine to be included in MDR-TB treatment regimens, thus providing hope for more effective therapeutic options for patients.
Tackling MDR-TB: The Significance of Cycloserine
The emergence of MDR-TB has posed a massive challenge to healthcare systems worldwide. MDR-TB is a form of TB that is resistant to at least two of the most potent first-line drugs, isoniazid and rifampin. This resistance complicates treatment and often requires the use of more toxic and less effective second-line drugs. Cycloserine has emerged as an essential player in this battle, given its unique mechanism of action and potential to be combined with other drugs to form a potent treatment regimen.
In this section, we will discuss the importance of cycloserine in the management of MDR-TB and its potential to revolutionize treatment strategies. We will also touch upon the challenges faced in implementing cycloserine-based treatment regimens and the ongoing efforts to optimize its use in clinical practice.
Optimizing Cycloserine Dosage and Regimens
One of the critical aspects of successfully treating MDR-TB with cycloserine is determining the optimal dosage and regimen. As with any antibiotic, striking the right balance between maximizing efficacy and minimizing toxicity is essential for ensuring patient compliance and long-term treatment success.
In this section, we will explore the various factors that influence the selection of the appropriate cycloserine dosage and regimen, including patient-specific factors, drug interactions, and the potential for dose optimization through therapeutic drug monitoring. We will also discuss the current recommendations and guidelines that inform the clinical use of cycloserine in MDR-TB treatment.
Addressing Cycloserine Side Effects and Toxicity
While cycloserine holds great promise in the management of MDR-TB, it is not without its challenges. Like many second-line drugs, cycloserine can cause a range of side effects, some of which can be severe or even life-threatening. These side effects include central nervous system (CNS) toxicity, psychiatric symptoms, and peripheral neuropathy, among others.
This section will focus on the potential side effects and toxicity associated with cycloserine use, as well as the strategies employed to mitigate these risks. We will discuss the importance of patient monitoring, dose adjustments, and the role of healthcare providers in ensuring the safe and effective use of cycloserine in MDR-TB treatment.
Overcoming Barriers to Cycloserine Access and Availability
Despite its potential as a valuable tool in the fight against MDR-TB, cycloserine remains relatively underutilized, primarily due to issues related to access and availability. Factors such as limited manufacturing capacity, high costs, and regulatory hurdles have created barriers to the widespread adoption of cycloserine in MDR-TB treatment regimens.
In this section, we will examine the various factors that contribute to the limited access and availability of cycloserine and discuss potential solutions and strategies to overcome these challenges. We will touch upon the role of international organizations, governments, and pharmaceutical companies in increasing the availability of cycloserine for patients in need.
The Future of Cycloserine in MDR-TB Management
As the global community continues to grapple with the challenge of MDR-TB, the role of cycloserine in treatment strategies is likely to evolve. Ongoing research and development efforts aim to enhance the efficacy, safety, and accessibility of cycloserine, thus paving the way for its more widespread use in MDR-TB management.
This final section will look at the future of cycloserine in MDR-TB management, including potential advancements in drug formulation, novel therapeutic approaches, and the role of global collaborations in driving innovation. We will also touch upon the importance of ongoing surveillance and research to ensure that cycloserine remains a viable and effective option in the ever-changing landscape of TB treatment.