HIV Medication & Birth Control Interaction Checker
This tool helps you determine if your HIV medications may reduce the effectiveness of your birth control method. Based on CDC and WHO guidelines, this checker provides personalized recommendations for safe contraceptive options.
When you're managing HIV with antiretroviral therapy, your life is already full of careful decisions: when to take pills, how to avoid drug interactions, how to stay healthy. But one of the most overlooked risks? Your birth control might not be working like you think it is.
Why Your Birth Control Might Be Failing
HIV protease inhibitors - drugs like lopinavir/ritonavir, a combination antiretroviral used to suppress HIV replication by blocking the virus’s ability to process proteins, or atazanavir, a protease inhibitor often boosted with ritonavir to increase its effectiveness - don’t just affect HIV. They mess with your hormones. Specifically, they interfere with how your body breaks down estrogen and progestin, the key ingredients in most birth control pills, patches, rings, and even implants.This isn’t theoretical. In a 2019 study published in The Lancet, women using the contraceptive ring (NuvaRing) while on efavirenz-based HIV treatment saw etonogestrel levels drop so low that 38% of them were no longer protected against pregnancy. That’s not a small risk. That’s a real chance you could get pregnant even if you never miss a pill.
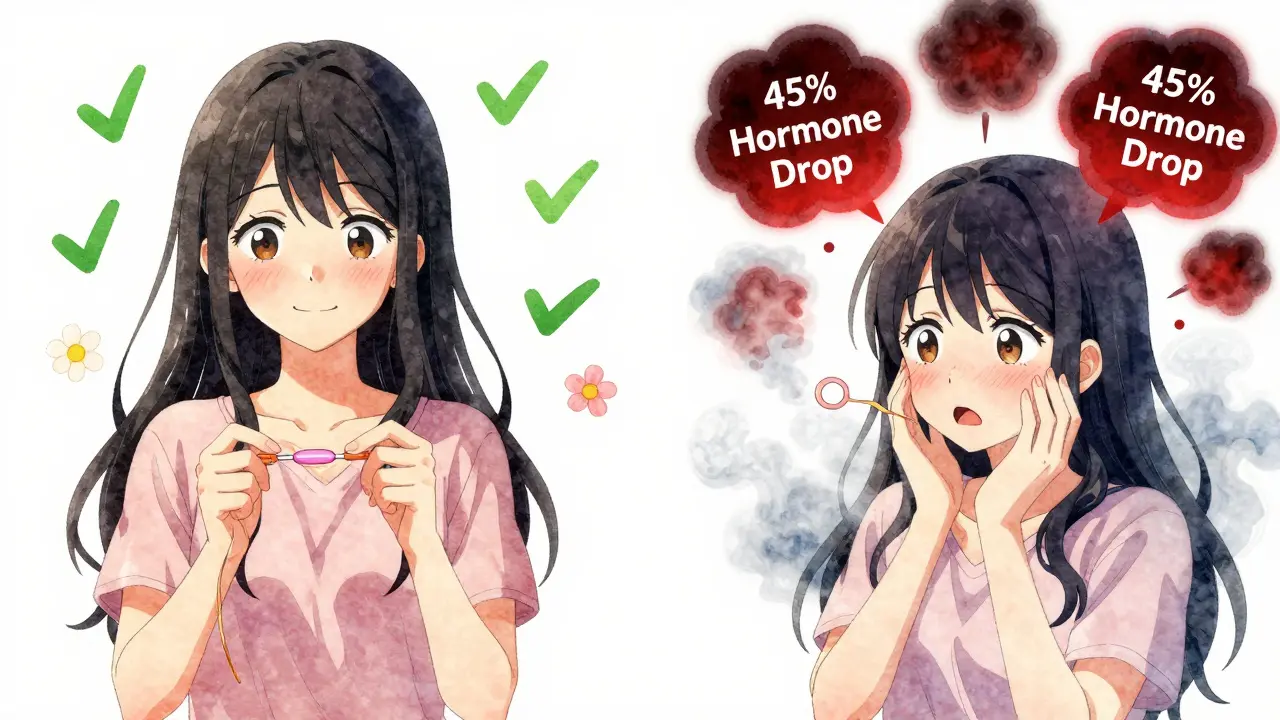
The problem? These drugs are strong inhibitors of the CYP3A4 enzyme - the same one your liver uses to clear hormones from your system. When protease inhibitors block this enzyme, they don’t always slow things down. Sometimes they speed them up. Or they change the balance between estrogen and progestin in unpredictable ways. One study found that when women took lopinavir/ritonavir with the contraceptive patch, ethinyl estradiol levels dropped by 45%. That’s a 45% drop in the hormone that prevents ovulation. Meanwhile, norelgestromin went up by 83%. That imbalance can lead to breakthrough bleeding, mood swings, and - worst of all - unintended pregnancy.
Which Birth Control Methods Are Riskiest?
Not all hormonal birth control is created equal when it comes to HIV drugs. Here’s what the data shows:- Combined oral contraceptives (COCs) - pills with estrogen and progestin - are the most vulnerable. Women on efavirenz-based regimens have pregnancy rates of 11-15%, compared to the typical 7-8% in HIV-negative women. Even with perfect use.
- Contraceptive patches and rings - both deliver hormones through the skin or vagina. But they’re just as affected by enzyme changes. The ring, in particular, has shown dramatic drops in hormone levels with efavirenz and some protease inhibitors.
- Progestin-only pills (mini-pills) - these are especially risky with ritonavir-boosted protease inhibitors. The World Health Organization (WHO) classifies this combination as Category 3 - meaning the risks usually outweigh the benefits. In simple terms: don’t use them together unless you have no other choice.
- Implants (like Nexplanon) - studies show ritonavir-boosted regimens can slash etonogestrel levels by 40-60%. That’s not just a reduction. That’s a near-total loss of protection.
Even depot medroxyprogesterone acetate (DMPA), the three-month shot (Depo-Provera), isn’t completely safe. While WHO still lists it as Category 1 (safe) with non-ritonavir regimens, real-world data from sub-Saharan Africa shows pregnancy rates jump to 12.3 per 100 woman-years when used with efavirenz - nearly double the rate seen with nevirapine.
What Actually Works?
The good news? There are options that don’t rely on your liver’s ability to process hormones.- Intrauterine devices (IUDs) - both hormonal (Mirena, Kyleena) and copper (Paragard) - are 99% effective, no matter what HIV drugs you’re on. They work locally in the uterus, so blood hormone levels don’t matter. This is the top recommendation from the CDC and WHO.
- Contraceptive implants - only if you’re on dolutegravir, an integrase inhibitor that has minimal interaction with hormonal contraceptives. New data from 2023 shows dolutegravir reduces etonogestrel levels by only 12%, which is not enough to compromise protection.
- Barrier methods - condoms, diaphragms, and spermicides - aren’t as effective as IUDs, but they’re safe and add protection against STIs, which is critical for people living with HIV.
One study from the University of California, San Francisco, found that 12 women chose to stop their HIV meds altogether just to keep using birth control pills. That’s how serious this is. You shouldn’t have to choose between staying healthy and preventing pregnancy.
What the Experts Say
Dr. Irene V. Bassett, who runs a clinic for HIV-positive women in Boston, has documented at least 17 cases of contraceptive failure in women using lopinavir/ritonavir with oral contraceptives - even when they took every pill on time. She says, “We’ve seen it too many times. It’s not about adherence. It’s about chemistry.”The CDC’s 2017 review of 32 studies concluded that the evidence for reduced effectiveness is strongest with efavirenz and ritonavir-boosted protease inhibitors. They recommend switching to non-hormonal methods whenever possible. The WHO agrees. In their 2015 guidelines, they explicitly say: if you’re on ritonavir-boosted PIs, avoid progestin-only pills.
And it’s not just about birth control pills. Emergency contraception (like Plan B) may also be less effective. A 2024 report from the National Institute of Child Health and Human Development found that levonorgestrel levels dropped by 35% in women taking darunavir/cobicistat - meaning the morning-after pill might not work at all.
Real Stories, Real Consequences
On HIV.gov’s forum, a woman named MariaJ wrote: “I took Tri-Sprintec every day for two years. I never missed a pill. I got pregnant. My doctor said it was the darunavir/cobicistat. I didn’t know that was even possible.”A 2021 survey by the Positive Women’s Network found that 28% of HIV-positive women had experienced contraceptive failure while using hormonal methods. Of those, 63% were on protease inhibitors. One Reddit user shared: “I used Depo-Provera with atazanavir/ritonavir. Got pregnant at 18 weeks. My OB said, ‘This happens. It’s documented.’ But no one told me before I started.”
These aren’t rare cases. They’re preventable.
What You Should Do
If you’re on HIV treatment and using hormonal birth control, here’s what to do now:- Check your HIV meds. Are you on a protease inhibitor? Ritonavir? Cobicistat? Darunavir? Lopinavir? Atazanavir? If yes, your birth control is likely compromised.
- Ask your provider: “Is my birth control safe with my HIV drugs?” Don’t wait for them to bring it up. Most clinicians still don’t screen for this routinely.
- Request an IUD. It’s the most reliable option. Insertion takes 10 minutes. It lasts 3-10 years. It doesn’t care what antiretrovirals you’re on.
- If you’re on dolutegravir, implants and IUDs are still your best bets. But oral pills? Maybe okay - but still not ideal.
- Use condoms. Always. They protect against STIs and add backup protection against pregnancy.
Healthcare providers need to do better, too. A 2022 survey found that 41% of HIV-positive women received no counseling on contraceptive interactions during their initial diagnosis. Community clinics were even worse - 28% less likely to provide this info than academic centers. That’s unacceptable.
The good news? Tools exist. The CDC has a free online interaction checker with 147 drug pairs. The American College of Obstetricians and Gynecologists recommends using the “teach-back” method: ask the patient to explain the plan in their own words. Patients who do this understand their options 85% of the time - compared to just 42% with regular counseling.
The Future Is Changing
The tide is turning. Dolutegravir is now the first-line HIV treatment for 72% of new patients - and it doesn’t interfere with birth control like protease inhibitors do. The WHO is expected to update its guidelines in 2025 to reflect this shift. By 2030, most HIV care will be integrated into one-stop clinics where contraception, HIV meds, and STI testing are all handled together.That’s progress. But for now, if you’re on a protease inhibitor, don’t assume your birth control is working. It might not be.
Can I still use the pill if I’m on HIV protease inhibitors?
It’s not recommended. Protease inhibitors like lopinavir/ritonavir, atazanavir, and darunavir - especially when boosted with ritonavir or cobicistat - can reduce hormone levels in birth control pills by up to 45%. This increases the risk of pregnancy, even if you take the pill perfectly. Progestin-only pills are especially risky and are classified as Category 3 by WHO. Switch to an IUD or implant instead.
Is the birth control implant safe with HIV meds?
It depends on the HIV drug. With ritonavir-boosted protease inhibitors, the implant’s hormone levels can drop by 40-60%, making it unreliable. But if you’re on dolutegravir or raltegravir, the drop is only around 12%, and the implant remains safe. Always check your specific drug combination with your provider before choosing an implant.
Why are IUDs recommended for women on HIV treatment?
IUDs work locally in the uterus - they don’t rely on hormones circulating in your bloodstream. That means HIV drugs can’t interfere with how they prevent pregnancy. Both copper and hormonal IUDs are 99% effective, no matter what antiretroviral regimen you’re on. They’re the most reliable, long-term option available.
Can emergency contraception (Plan B) still work with HIV drugs?
It might not. Studies show that darunavir/cobicistat reduces levonorgestrel levels by 35%, which could make Plan B ineffective. If you need emergency contraception and are on a protease inhibitor, ask your provider about ulipristal acetate (Ella) or a copper IUD - both are more reliable in this situation.
How do I know if my HIV meds interact with my birth control?
Use the CDC’s free online interaction checker, which lists 147 drug combinations. You can also ask your pharmacist or HIV provider to run your specific meds through it. If you’re on ritonavir, cobicistat, efavirenz, or any protease inhibitor, assume your hormonal birth control is affected until proven otherwise.